Neoplastic Lumbosacral Plexopathy in Untreated Cervical Cancer: A Case Report
Article information
Abstract
In this report, we present the case of a patient with cervical adenocarcinoma with progressive right lower-extremity pain and weakness. Electromyography of the lower extremities and subsequent ultrasonographic imaging complementarily demonstrated findings considered suspicious for the perineural spread of malignancy to the lumbosacral plexus and sciatic nerve. This possibility was confirmed by magnetic resonance imaging (MRI) and fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) scanning. This case report suggests that in addition to MRI and FDG PET/CT scans, electromyography and ultrasonographic imaging are valuable modalities for the diagnosis of perineural malignancy.
Introduction
Although the morbidity of cancer is increasing, its involvement in the peripheral nervous system is relatively uncommon. In particular, neoplastic lumbosacral plexopathy (NLP), which typically manifests as painful neuropathy, is a rare complication that is generally associated with prostate cancer.
According to a previous study, the frequency of cancer metastasis to the lumbosacral plexus is 0.71% [1]. Another research reported the incidence of histologically confirmed parametrial perineural invasion as 7.53% in early-stage cervical cancer patients and that of perineural invasion as 12.5% in the cervical stroma [2,3]. The prevalence of NLP may have been underestimated in previous studies. Therefore, a thorough investigation of metastatic neural invasion is needed.
Computed tomography (CT) or magnetic resonance imaging (MRI) scans are commonly considered as the initial modalities to diagnose NLP [4]. However, these modalities are expensive, and the radiation exposure during CT scans cannot be ignored. In this report, we discuss the case of a patient who was diagnosed with NLP and suggest electromyography (EMG) and ultrasonography as cost-effective and less invasive tools for the early diagnosis of NLP.
Case Report
A 40-year-old female patient complained of rapidly progressive right lower-extremity pain and weakness that had developed over approximately 5 months. Although the patient had been diagnosed with micro-invasive cervical squamous cell carcinoma 1.5 years previously, she declined further examinations and appropriate treatment, such as chemoradiation therapy. Approximately 1 year after the initial diagnosis, the patient started to experience pain, hypoesthesia, and weakness in the right hip and leg. She chose alternative medicine preferentially and received honey bee venom needle therapy for 6 months. However, the symptoms were not relieved; thus, the patient visited a pain clinic and was diagnosed with lumbar disc herniation based on MRI and underwent disc decompression and percutaneous epidural neuroplasty with ballooning; however, this did not alleviate her pain. Finally, she experienced right foot drop and visited our clinic for an examination.
The initial physical examination revealed that motor function was 0 in both flexors and extensors of the right ankle and toes and poor in the knee flexors and the hip extensors. Motor strength was normal in the other limbs. Hypoesthesia was observed from the right posterior and medial leg to the foot. Vibration sensation and joint positioning of the right toes were diminished. The right ankle reflex was absent. Upper motor neuron signs, including the Babinski sign, were not evident. The patient did not have any urinary or bowel symptoms.
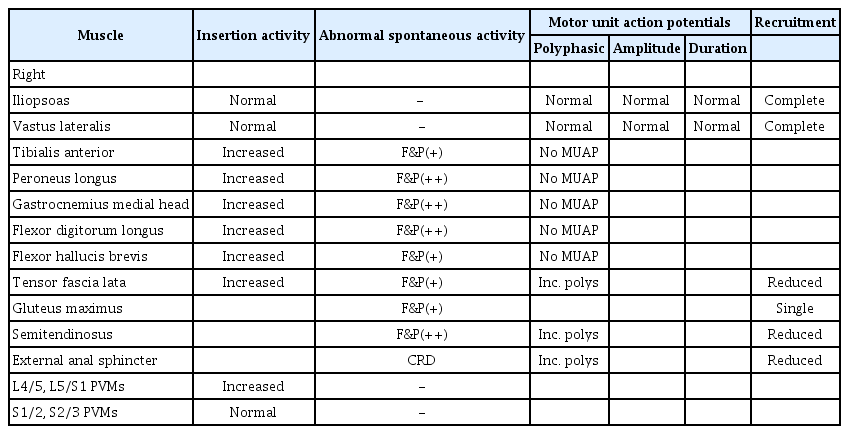
An electrophysiological study suggested severe right multiple lumbosacral radiculoplexopathy from the L5–S4 roots with considerable involvement of the sciatic nerve (Table 1). Nerve conduction studies demonstrated the absence of a motor response from the peroneal and tibial nerves and the absence of a sensory response from the sural nerve in the right lower limb.
On ultrasonography, a remarkably enlarged right sciatic nerve was identified from the gluteal fold to the thigh (Fig. 1A, B). MRI of the pelvis revealed enlargement of the right lower lumbosacral plexus from the L5–S3 nerve roots to the right sciatic nerve (Fig. 1C). A subsequent fluorodeoxyglucose positron emission tomography/CT (FDG PET/CT) scan demonstrated linear asymmetric hypermetabolic activity in the right pelvis, compatible with swelling of the lumbosacral plexus identified on MRI (Fig. 1D). These findings suggested neural metastases from the L5–S3 nerve roots along the right sciatic nerve.
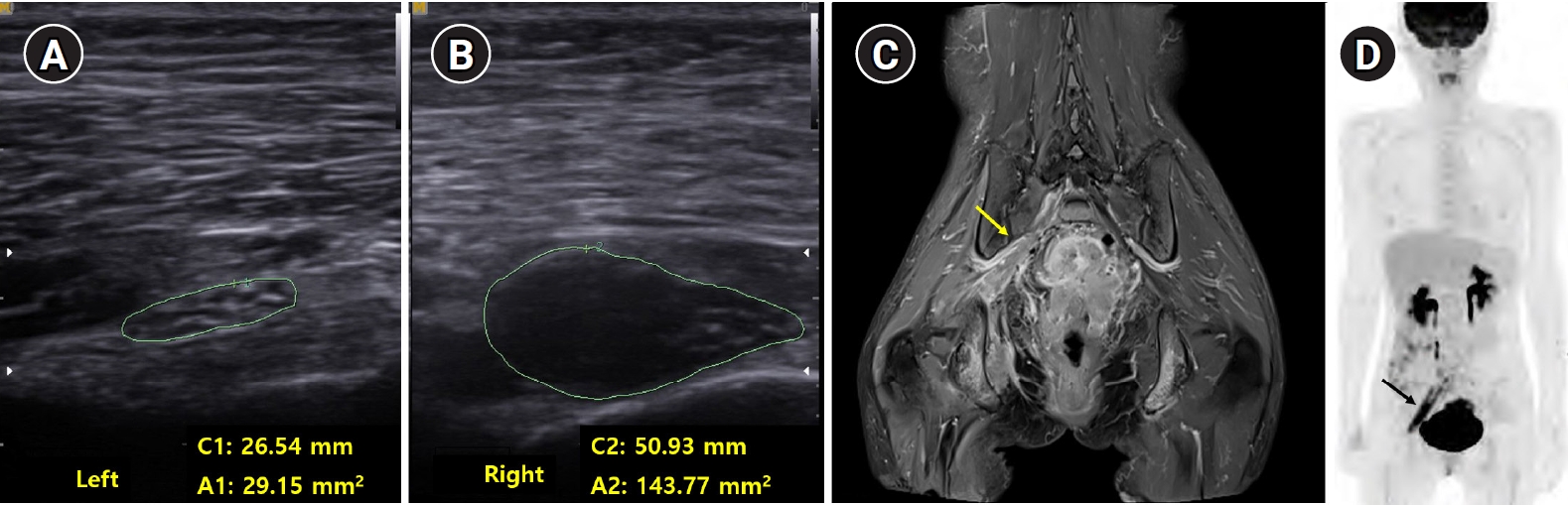
(A, B) Cross-sectional ultrasonographic image of bilateral sciatic nerve. The area of the sciatic nerve is significantly larger on the right-side (B) than on the left-side (A). C1, C2, circumferences of the sciatic nerve; A1, A2, areas of the sciatic nerve. (C) Magnetic resonance imaging (MRI), (D) Fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) images of sciatic nerve. (C) The right lumbosacral plexus (yellow arrow) is remarkably enlarged with a low-signal mass in MRI. (D) Linearly increased FDG uptake (black arrow) is found in the right pelvis on PET/CT.
The patient was clinically diagnosed with stage III C1 cervical cancer (5.4 cm × 5.7 cm × 6.3 cm) with invasion of the right pelvic wall and multiple lymph node metastases. She started concurrent chemoradiation therapy (CCRT) using a cisplatin and 5-fluorouracil regimen and external beam radiation of 63.7 Gy. After completion of 3 cycles of CCRT, the cancer showed partial regression on MRI, and the motor function in the right knee flexors and hip extensors improved from poor to good. However, the foot drop did not show significant improvement.
In a follow-up EMG study, decreased insertional activities with no motor unit action potential were noted in the right tibialis anterior, peroneus longus, gastrocnemius medial head, biceps femoris short head, and tensor fascia lata muscles, and there was no significant interval change.
Discussion
NLP results from the direct neural invasion of tumors or other metastatic diseases. Based on previous studies, the perineural spread of malignancy progresses through the direct infiltration of the perineural space, instead of via lymphatics. Pelvic malignancies, such as uterine, prostate, and rectal cancers, are common causes of NLP. Local perineural invasion can also occur in patients with cervical cancer and has a poor prognosis. Invasion of cervical adenocarcinoma and cervical epidermoid cancer to the sacral nerve roots occurs by a mechanism similar to that of prostate cancer spreading to the sciatic nerve [5].
The innervation of the uterus and the cervix has been defined well in gynecology owing to the development of nerve-sparing surgery, and a direct neural pathway to the sciatic nerve has been discovered. Lateral to the uterosacral ligament, the hypogastric plexus provides both sympathetic and parasympathetic nerves to the uterus, bladder, and rectum [6]. The splanchnic plexus, which originates from the S2–S4 roots, provides sympathetic innervation. The entire sciatic nerve and lumbosacral plexus become prone to metastases after cancer invades the S2–S4 roots.
In this patient with untreated cervical cancer, the EMG study suggested right severe multiple lumbosacral plexopathy from the L5–S4 roots with severe involvement of the sciatic nerve. Subsequent ultrasonographic imaging also demonstrated significant swelling of the right sciatic nerve. Therefore, considering the clinical history of cervical cancer, along with the electrophysiological and ultrasonographic findings, a metastatic lesion of the right lumbosacral plexus was suggested. Finally, MRI demonstrated an asymmetrical linear thickening, which was supported by increased FDG activity in the PET/CT scan, reflecting the L5–S3 nerve roots and right sciatic nerve invasion.
Frequently, neuropathy or neuritis due to chronic radiation can be incorrectly diagnosed as the perineural spread of malignancy; since the majority of pelvic cancer patients receive radiation therapy, a careful differential diagnosis is important. Thomas et al. [7] compared 20 cases of radiation neuropathy and 30 cases of malignant lumbosacral plexopathy. The radiation neuropathy group reported weakness and numbness as the most common symptoms; however, for the NLP group, pain was the chief complaint.
On EMG, myokymic discharges are frequently observed in patients with radiation-induced neuropathy or plexopathy patients; thus, these discharges are an important electrophysiological characteristic of radiation injury [8]. In this case, no myokymic discharge was observed on EMG. Malignant neuropathy can also be distinguished from radiation neuritis based on MRI. Radiation neuritis is usually restricted to the radiation area and typically shows a thin peripheral “tram–track” pattern of enhancement without irregularity [9]. Concurrently, when the perineural spread of malignancy occurs, it presents comparatively thicker enhancement around the individual nerves and may be asymmetrical, as in the patient in this study [10].
In conclusion, intraneural metastasis in the lumbosacral plexus caused by malignancy is a rare condition, and the majority of cases occur in patients with prostate cancer. In this study, a patient with untreated cervical cancer who experienced lower-extremity weakness and pain was finally diagnosed with neural metastases after several procedures. The study revealed that in addition to MRI and FDG PET/CT scans, EMG and ultrasonographic imaging can be relevant modalities for the diagnosis of perineural malignancy.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.