근전도를 이용한 신경내 결절종에 의한 족하수의 조기진단 및 성공적 치료
Early Diagnosis with Electrodiagnostic Study and Successful Treatment of Foot Drop Caused by Intraneural Ganglion cyst
Article information
Trans Abstract
Foot drop is a commonly encountered symptom in electrodiagnostic lab. It is uncommon for peroneal nerve to be compressed by ganglion cyst around the fibular head, but it is important to differentiate peroneal lesion from lumbar radiculopathy which occurs more often. With treatment followed by prompt and exact diagnosis, we can minimize motor weakness due to nerve damage. We report a case in which a 60-year-old woman who complained of right foot drop was diagnosed with peroneal nerve palsy caused by intraneural ganglion cyst around the fibular head. In comparison with other case reports about peroneal nerve palsy caused by ganglion cyst, the diagnosis of this case was made immediately after onset of the foot drop by electromyogram and the patient recovered from motor weakness after surgery.
Introduction
Foot drop is a common symptom encountered by physiatrists in the electrodiagnostic lab. Lesions causing the foot drop could arise from the anterior horn cell at the lumbar spinal cord through lumbosacral plexus to the peroneal nerve. Physiatrists should differentiate foot drop caused by lumbar radiculopathy from peroneal nerve palsy. The former would have a chronic course and often involve back pain and radiating pain on lower extremity, while the latter may have a sudden onset by trauma or may occur with pain and mass around the fibular head. Since the anatomical characteristic of the peroneal nerve, which winds around the fibular head and divides into the superficial peroneal nerve (SPN) and deep peroneal nerve (DPN) from the common peroneal nerve (CPN)¹, foot drop can occur by lesion around the fibular head. Intraneural or extraneural ganglion cyst around the fibular head can cause foot drop, but its prevalence is very rare.2 This is why it is difficult to diagnose peroneal nerve lesion around the fibular head. We report a case of early diagnosis of peroneal nerve palsy due to intraneural ganglion cyst around the fibular head using electrodiagnostic test, which resulted in successful motor recovery.
Case
A 60-year-old woman visited the local medical center because of sudden onset of right foot drop. Magnetic resonance imaging (MRI) revealed mild lumbar spinal stenosis. She was referred to the emergency room (ER) for further evaluation and management 3 days after onset of symptoms. She had a medical history of diabetes mellitus, hypertension, and Graves’ disease and had undergone bilateral total knee replacement 5 years prior. She denied history of any trauma. The primary physician and neurosurgeon suspected lumbar radiculopathy as the cause of her symptom. However, there was no evidence of any root compression or spinal cord injury on MRI, and she did not complain of any low back pain or sciatica. Computed tomography (CT) of the right lower extremity did not show any suspicious lesions. For evaluation of her foot drop, she was referred to the Department of Rehabilitation Medicine for nerve conduction study (NCS) and electromyography (EMG) during admission in the ER.
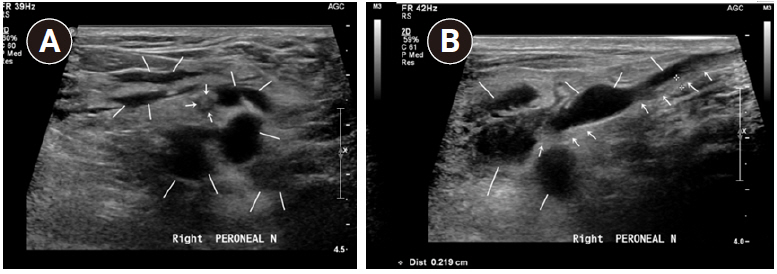
Manual muscle test (MMT) for grading of strength revealed a score of 1/5 on right ankle dorsiflexion, 2/5 on ankle eversion, and 1/5 on extension of the great toe and the other toes. Hypoesthesia on the 1st dorsal webspace of the right foot was also noted. There was a palpable mass around the right fibular head, and Tinel’s sign was positive. To localize the lesion, EMG was performed 3 days after the onset of the symptoms (Table 1).
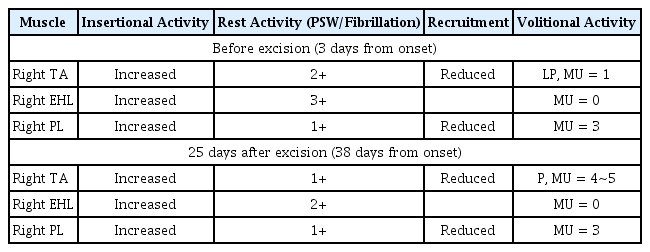
Compound motor action potentials (CMAPs) of the right DPN revealed that there was a 55% conduction block of the amplitude across the fibular head and 45.9% of axon loss compared to that in the CMAPs of the left DPN. Sensory nerve action potentials (SNAPs) of the right SPN showed normal range of latency and amplitude (3.03 msec, 15.2 μV), same as the left superficial peroneal sensory nerve (3.1 msec, 13.8 μV). Deep peroenal sensory conduction study was not done. EMG of the right TA and PL showed increased insertional activity with some positive sharp waves and fibrillations at rest and decreased recruitment of motor units with long duration and increased polyphasic patterns on volition (Table 2). Ultrasonography revealed a multiseptated cystic mass along the right CPN around the right fibular head (Fig. 1).
A cystic mass (solid white line) around the right fibular head along with peroneal nerve (white arrow) is shown. A) axial view, B) longitudinal view.
Since the lesion to cause conduction block of the peroneal nerve was suspected, the physiatrist recommended to arrange operation of excision of the cyst immediately. However, the operation was delayed for 10 days after the diagnosis because of the risk of thyrotoxicosis and poor control of the blood sugar levels. To minimize muscle atrophy, she was prescribed electrical stimulation therapy (EST) on right TA, EDL, and PL. To prevent heel cord tightness, ankle-foot-orthosis (AFO) and stretching exercise for the Achilles tendon were prescribed. The operation was performed 13 days from the onset of the symptoms. In the operative field, a bulging cyst was found on the fascia as well as the cystic mass inside the nerve sheath along the CPN. No atrophic change was seen on the nerve. The cyst was dissected from the nerve, revealed as ganglion, previously fragmented, filled with mucoid yellow fluid, 1.3g in weight, 7.6×1.3×0.2cm in dimensions for the largest one.
Twenty-five days after excision of the cyst, MMT improved to 3/5 on the right ankle dorsiflexor from 1/5 initially. The CMAP of the right DPN showed decreased amplitude compared to that in the first EMG. The axon loss progressed to 94.8% compared with 45.9% initially, and the conduction block was not demonstrated. EMG of the right TA also showed 4 to 5 motor units recruited on volition compared with only 1 at the first study (Table 2). EMG of the right EHL and PL showed no recovery. After 38 days from onset, she was able to walk without foot drop. Follow-up EMG was to be performed when axonal regeneration was suspected to take place. However, she did not visit the hospital.
This study was approved by the Institutional Review Board for the exemption of written informed consent (IRB number:H-1902-011-076).
Discussion
This study reported a case of sudden onset of right foot drop. Since the patient was referred to department of rehabilitation medicine to perform NCS and EMG during admission in the ER, peroneal nerve palsy around the fibular head could be diagnosed by EMG. It helped the physician to perform early intervention, which was fundamental to preventing permanent gait abnormality.
Owing to low prevalence of peroneal nerve palsy caused by intraneural or extraneural ganglion cyst, it is not easily diagnosed.2 One study revealed that the prevalence of ganglion cyst at the proximal tibiofibular joint (PTFJ) was only 0.76%.3 With low prevalence of the ganglion cyst involving the peroneal nerve, a misdiagnosis can easily be made.
To detect ganglion cysts, MRI is preferred as it provides good contrast of soft tissue.4 However, in this case, MRI was not done because the patient had undergone total knee replacement. Metallic artifact was suspected to limit cyst detection. Because of limitation in demonstrating soft tissue contrast, CT was not useful. Hence, electrodiagnostic test and ultrasonography were the next choices. Electrodiagnostic test is one of the most useful diagnostic tools to reveal any radiculopathy or peripheral neuropathy without exposure to radiation or invasive techniques. It can localize the lesion effectively combined with ultrasonography as useful as MRI for soft tissue lesion.
Most case reports claim that surgical dissection is the treatment of choice and that it reduces the rate of recurrence. As the ganglion cyst is considered to arise from the PTFJ, it is important to completely dissect the base of the stalk from its origin.5 Excision should ideally be performed between 3 and 4 months after the onset.4 In a recent study, the outcome of surgical excision of peroneal neuropathy revealed a trend toward greater improvement with shorter time to surgery.6
Several reports about peroneal nerve palsy owing to ganglion cyst report misdiagnosis and delayed treatment. In one study, a 45-year-old man complained of right foot drop with a 2-month history and was diagnosed via MRI and EMG and got surgical excision to regain full motor recovery after 4 months. For this case, tenderness and gradual development of swelling around the fibular head were noted.4 In another case, a 57-year-old man with acute lower limb pain and sudden foot drop visited a clinic and misdiagnosis made him revisit after 4 weeks with no clinical improvement. EMG and MRI of left knee revealed a cystic lesion at the fibular head and he gained almost full recovery of muscle function at 2 months postoperatively.7 In these two cases, the ganglion cyst causing foot drop was an extraneural lesion. Obvious mass with pain around the fibular head could lead physicians to diagnose lesion around the fibular head However, we usually encounter more common symptom such as motor weakness and numbness in the lateral aspect of lower extremity, as seen in the latter study. As many patients often involve degenerative disc disease of lumbar spine, it is more ambiguous to diagnose individual nerve lesion from root lesions.
The difficulty in differential diagnosis of peroneal nerve palsy from lumbar radiculopathy is also seen in another report. A 69-year-old woman with no history of trauma complained of right foot drop with intermittent radiating pain to the right calf. Misdiagnosis was made as lumbar radiculopathy and it took 5 months until diagnosis and surgical excision of intraneural ganglion cyst around her fibular head was made. Her motor function did not recover at 6 months postoperatively.8 In our case, the patient was diagnosed as early as 3 days after onset and underwent surgery 13 days after onset, the fastest intervention among similar cases. With negative radiologic findings in the ER, she was referred to the EMG room and prompt diagnosis was made.
It is not well known whether there is a difference between intraneural and extraneural lesions regarding their effect on nerve damage and recurrence. Intraneural cyst would consistently compress the nerve fiber inside the nerve sheath, could resulting in permanent nerve damage. In contrast, nerve compression owing to extraneural lesion might be not inconsistent, resulting in less axonal damage. Compared to the intraneural case with no recovery8, the first two extraneural cases showed complete motor recovery despite the delay in surgical intervention.4,7 In our case report, she was able to walk after 1 month because of early diagnosis by EMG.
Conclusion
As ganglion cyst in the lower extremity is very rare, the diagnosis of the ganglion cyst around the fibular head would have been very difficult. However, proper history taking, physical examination, EMG as well as appropriate imaging tool helped in accurate and immediate diagnosis. Early diagnosis with EMG in this case report made early intervention possible and the patient could recover from permanent motor weakness.
Acknowledgements
We thank Dr. Hong, who is a surgeon of Orthopedics at Bone Barun Hospital, for providing information on the surgery and Dr. Song, a professor of the Department of Radiology of Pusan National University Hospital for providing information of ultrasonographic finding.