Introduction
The flexor pollicis longus (FPL) muscle is innervated by the anterior interosseous nerve (AIN), median nerve (MN), lateral-medial cords, middle-lower trunks, and C7-C8-T1. The FPL functions as a flexor of the interphalangeal joint of the thumb [
1]. This muscle is used for needle electromyography (EMG) in AIN syndrome or proximal median neuropathy. Notably, the FPL is characteristically spared in cases of carpal tunnel syndrome [
2].
The FPL, flexor digitorum profundus (FDP) 1 and 2, and pronator quadratus (PQ) innervated by the AIN are used in the diagnosis of isolated AIN neuropathy or proximal median neuropathy. According to Goodmurphy et al. [
3], the accuracy of the FDP (66.7%), FPL (14.3%), and PQ (35.7%) was not high when needle EMG examinations were performed using the blind technique. Notably, regarding the FDP, the needle was located in FDP 3 and 4, which are innervated by the ulnar nerve, and damage to the radial artery (RA) was observed [
3].
Examining the AIN in muscles is challenging because of its deep location and small size. In previous studies, safe and accurate needle insertion positions were reported using ultrasound for the PQ and FDP 1 and 2, and for the PQ, safety was confirmed in cadaveric studies [
4-
6].
The method used for the FPL varies depending on the author. Some authors have described a technique for inserting a needle between the flexor carpi radialis (FCR) and brachioradialis (BR) muscles at the distal third of the forearm while the forearm is in a supinated position [
7,
8]. Perotto [
9] presented a method of penetrating the FCR and flexor digitorum superficialis (FDS) by inserting a needle into the volar side of the radius in the middle of the forearm.
However, locating the BR at the one-third mark of the forearm is difficult because it has no landmarks. Moreover, predicting the depth of entry into the FDP through the FCR and FDS in the mid-forearm is complex. Furthermore, since the path of needle entry in the distal third of the forearm would involve the RA, superficial branch of the radial nerve, and radial nerve, whether needle insertion in this area is safe for neurovascular structures is a matter of debate.
This study analyzed the anatomical relationship between the MN, RA, and FPL muscles using ultrasonography based on the FCR tendon. Additionally, to overcome the limitations of the existing method, we present a new method of using the FCR tendon as a landmark.
Materials and Methods
1) Participant recruitment
This study examined 56 upper extremities of 28 healthy adults (15 men and 13 women) using ultrasound (Accuvix V20 with 5 to 13 MHz; Samsung Medison, Seoul, Korea). Participants with a forearm injury, a history of surgery, or a diagnosis of upper-extremity neuropathy were excluded. Data regarding the sex, age, height, weight, and body mass index of the participants were recorded.
All participants provided informed consent for the publication of their clinical details. This study was approved by the Institutional Review Board of Korea University Ansan Hospital (No. 2021AS0050).
2) Ultrasonographic examinations
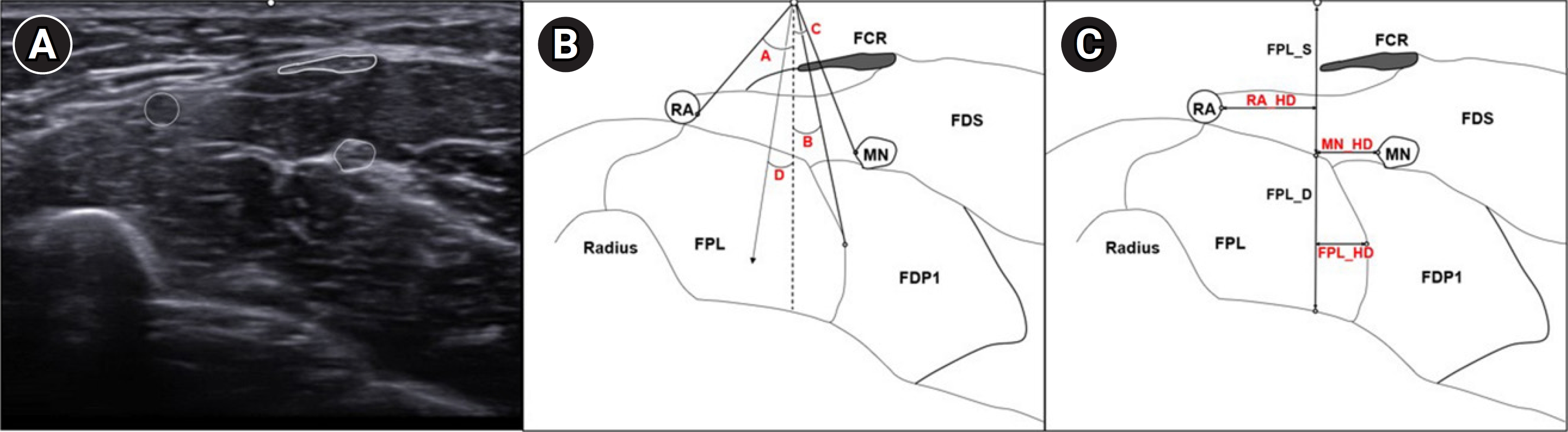
In the forearm supination state, the examination was performed at the distal one-third point at the line joining the medial epicondyle and ulnar styloid process (
Fig. 1A). The radial side of the FCR tendon was defined as the insertion point (IP) of the needle. A vertical line (VL) descending vertically from the IP was defined. Angle A was defined as the angle between the VL and ulnar sides of the RA. Angle B was defined as the angle between the radial margins of FDP1 and VL. Angle C was defined as the angle between the radial sides of the MN and VL. Finally, the average value of angles A and B was considered angle D (
Fig. 1B).
The horizontal distance between the VL and RA was then measured and named RA_HD. Next, the horizontal distance between the VL and MN was measured and named MN_HD. Finally, the horizontal distance of the radial margins of the VL and FPL was measured and named FPL_HD. A negative value for an angle was defined as being radial to the VL (
Fig. 1C).
Results
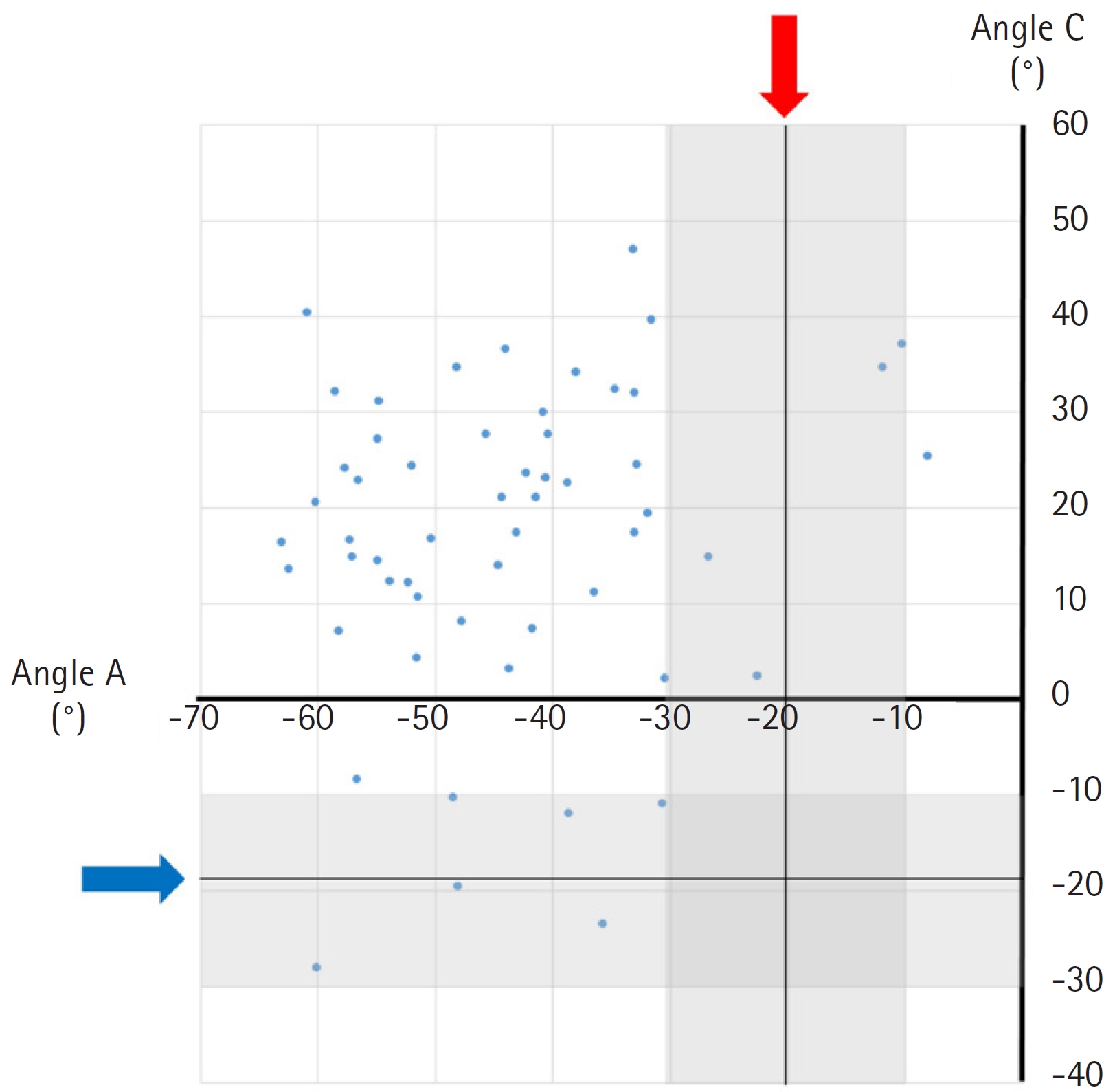
The measurement values are presented in
Table 1. The median values of angles A, B, C, and D were -44.3° (minimum, -63.1°; maximum, -8.1°), 4.0° (minimum, -23.7°; maximum, 32.3°), 18.5° (minimum, -28.0°; maximum, 47.0°), and -19.8° (minimum, 41.9°; maximum, 11.0°), respectively.
Meanwhile, the median values of RA_HD, MN_HD, and FPL_HD were -6.0 mm (minimum, -11.0 mm; maximum, -0.8 mm), 3.9 mm (minimum, -5.3 mm; maximum, 9.2 mm); and 1.8 mm (minimum, -5.7 mm; maximum, 8.8 mm), respectively.
Fig. 2 is a scatter plot demonstrating angle A on the x-axis and angle C on the y-axis. An angle at -30° to -10° was considered the safety zone based on the median value of angle D (-19.8°). In the safety zone, four cases (7.1%) overlapped with angle A, and six cases (10.7%) intersected with angle C.
RA_HD had negative values, and the RA was always located on the radial side of the IP. Both MN_HD and FPL_HD were present on the radial and ulnar sides of the IP.
Discussion
EMG was relatively well tolerated and had no significant side effects. However, because needle EMG examination is an invasive procedure, there is a risk of bleeding, infection, and nerve injury under certain circumstances [
10]. Because the FPL has a deep location and contains neurovascular structures such as the MN and RA, inserting the needle requires caution. Nevertheless, no studies have previously been conducted to verify the safety of the existing method.
Ultrasound imaging is a noninvasive technique that enables real-time examination of nerves, blood vessels, and muscles. This method allows for direct assessment of both the needle and the target muscle, allowing safe needle insertion [
11]. However, ultrasound-guided insertion is time-consuming and necessitates the use of specialized equipment.
Therefore, a safe and accurate technique for needle insertion without imaging guidance is required. Unfortunately, the existing methods are ambiguous because no unmistakable landmarks exist. This study presents a novel needle insertion method using the FCR tendon as a landmark. Because the FCR tendon does not have anatomical variations, such as those seen with the palmaris longus tendon, it can be used as a landmark in almost any situation. However, in our study, the distribution of locations was heterogeneous due to anatomical variations in the RA and MN.
Our results confirmed that the RA or MN could be damaged within a range of 10° based on angle D, and this information could be used to secure a safe distance from the MN and RA. Moreover, the distribution of the FPL or MN varied on the radial or ulnar sides based on the IP. Thus, accurately inserting the needle into the FPL was difficult.
In our method, the probability of RA puncture was 10.7%, and the likelihood of MN puncture was 7.1%. Although directly comparing our method with those presented in the literature was not possible, our method can be considered relatively safe. If the needle enters slowly, the RA may slip and be avoided. Moreover, injury to the MN can be avoided if the needle is withdrawn as soon as the patient complains of tingling.
However, an FPL examination without imaging guidance poses a non-trivial risk of neurovascular injury.
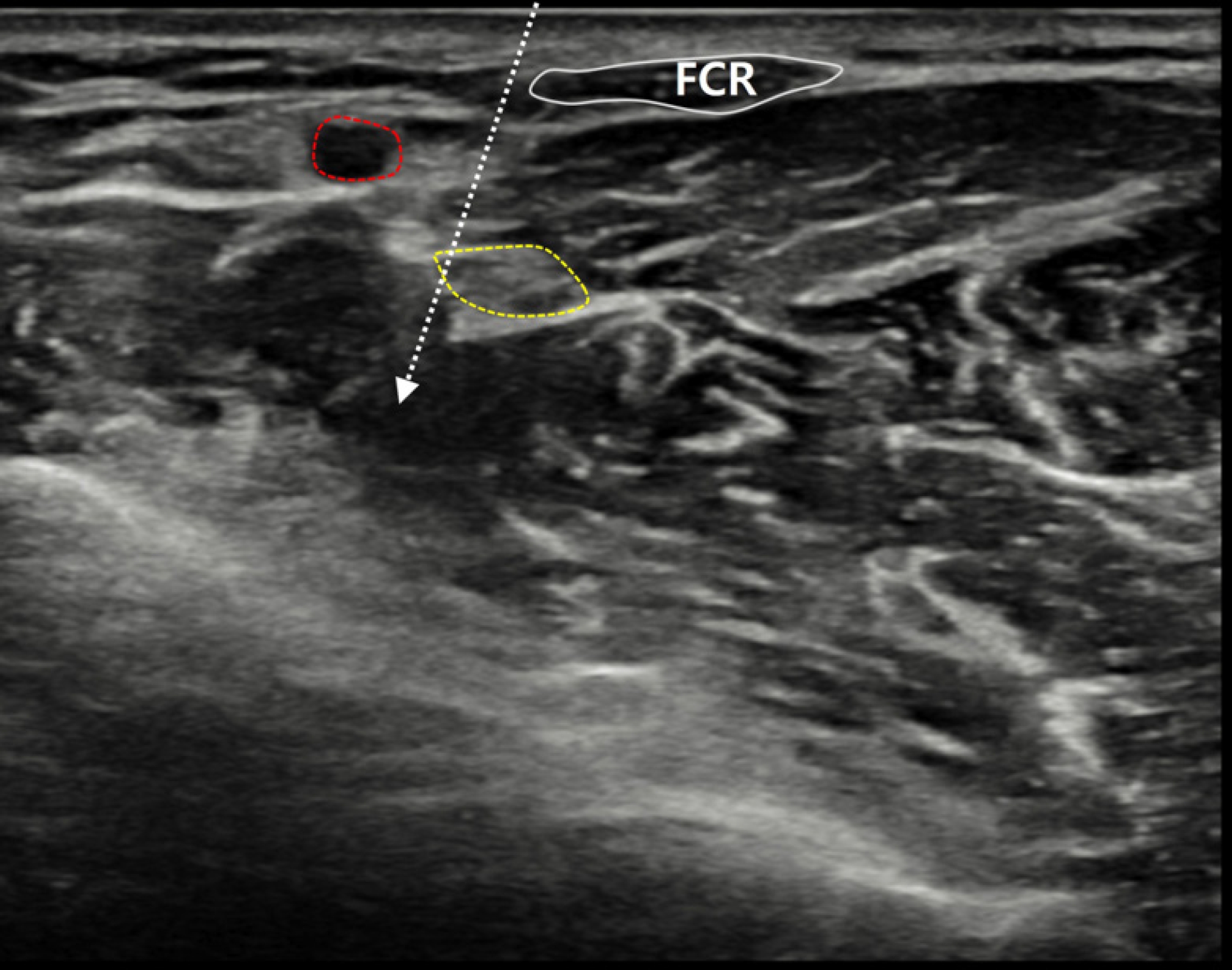
Fig. 3 presents a case where the MN was located in the trajectory of the needle. Conducting the examination using ultrasound may be preferable in terms of safety.
However, our study has some limitations. First, our study did not rigorously compare the safety profile with that of previous research. Second, even if the examiner presses the ultrasound probe with minimal force, movement of the internal structure may occur as pressure is applied.
In conclusion, this study proposed a new method for examining the FPL that uses the FCR tendon, which does not have anatomical variations, as the anatomical landmark. Although a direct comparison with the existing method was not possible, we found a relatively low probability of RA puncture (10.7%) and MN puncture (7.1%). In addition, we believe that advancing the needle slowly and withdrawing the needle as soon as the patient complains of discomfort minimizes the possibility of nerve injury. Nevertheless, this technique without imaging guidance still has a low probability of neurovascular injury. Therefore, we recommend using ultrasound when examining the FPL, and the method proposed in this study should be used as an alternative if ultrasound imaging is not available.
Conflict of Interest
Dong Hwee Kim is an editor-in-chief of the journal. But he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Fig. 1.
Cross-sectional sonogram (A) and schematic drawing (B, C) demonstrating the relationship of the lateral border of the flexor carpi radialis (FCR) tendon (black arrows) with the median nerve, flexor pollicis longus (FPL), and radial artery. Negative values in are shown for angles A, B, and C, and the horizontal distances are lateral to the vertical line. A, angle between the vertical line and radial artery; B, angle between the vertical line and medial margin of the FPL; C, angle between the vertical line and median nerve; D, middle angle between the radial artery and FPL medial margin calculated as the sum of A and B, divided by 2; RA_HD, horizontal distance from the vertical line at the lateral margin of the FCR tendon to the radial artery; MN_HD, horizontal distance from the vertical line at the lateral margin of the FCR tendon to the median nerve; FPL_HD, horizontal distance from the vertical line at the lateral margin of the FCR tendon to the medial border of the FPL. FDS, flexor digitorum superficialis; FDP, flexor digitorum profundus.
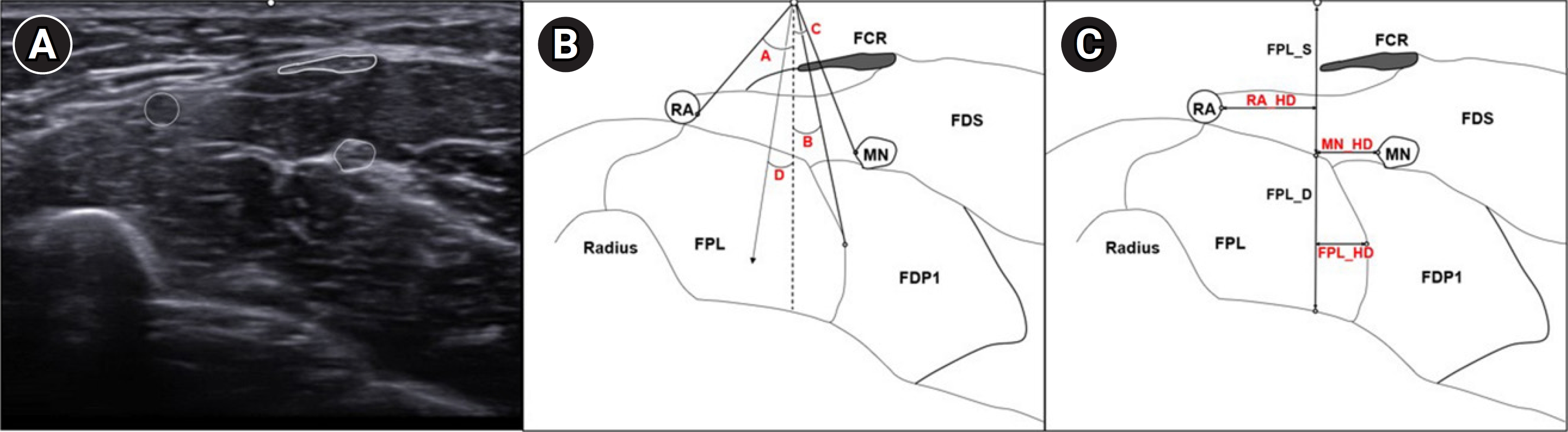
Fig. 2.
Scatter plot demonstrating the relationship between angle A (radial artery) on the x-axis and angle C (median nerve) on the y-axis. Considering angles in the range of -30° to -10° based on the median value of angle D (-19.8°) as the safety zone, four cases (7.1%) overlapped with angle A, and six cases (10.7%) intersected with angle C.
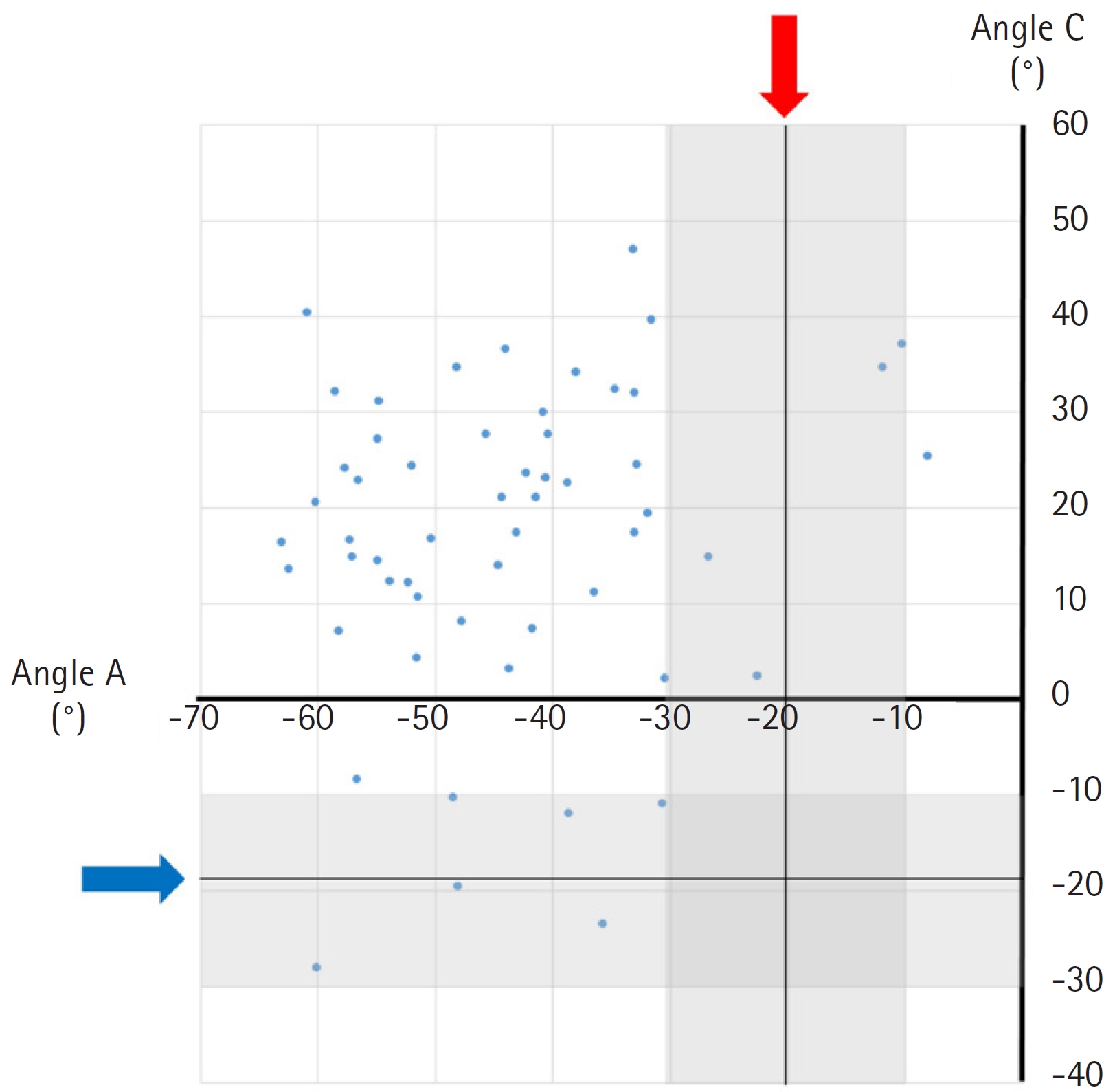
Fig. 3.
Short-axis ultrasonography view of the distal third of the forearm. The red circle indicates the radial artery. The yellow circle indicates the median nerve. The white dashed arrow demonstrates the trajectory of the needle. The white dashed arrow is in contact with the yellow circle. FCR, flexor carpi radialis.
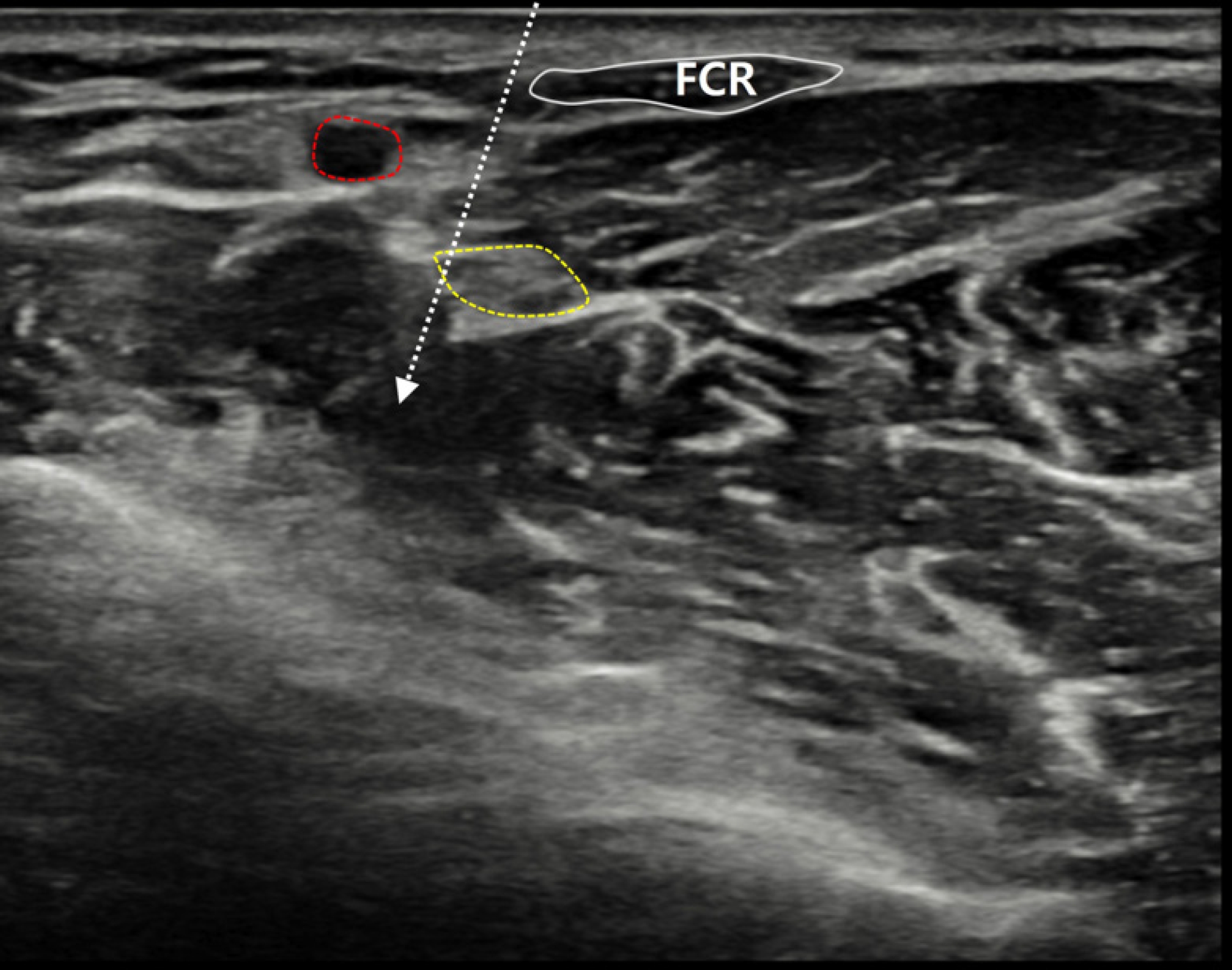
Table 1.
Anatomical Parameters of the Flexor Pollicis Longus
|
Parameters |
Median |
Minimum |
Maximum |
|
Angle A (°) |
−44.3 |
−63.1 |
−8.1 |
|
Angle B (°) |
4.0 |
−23.7 |
32.3 |
|
Angle C (°) |
18.5 |
−28.0 |
47.0 |
|
Angle D (A+B/2) (°) |
−19.8 |
−41.9 |
11.0 |
|
RA_HD (mm) |
−6.0 |
−11.0 |
−0.8 |
|
MN_HD (mm) |
3.9 |
−5.3 |
9.2 |
|
FPL_HD (mm) |
1.8 |
−5.7 |
8.8 |
|
FPL_S (mm) |
10.8 |
6.6 |
15.6 |
|
FPL_D (mm) |
20.7 |
16.0 |
26.2 |
References
1. Jenkins DB, Hollinshead WH: Hollinshead’s functional anatomy of the limbs and back. 9th ed. St. Louis: Saunders/Elsevier; 2009.
2. Preston DC, Shapiro BE: Electromyography and neuromuscular disorders: clinical-electrophysiologic-ultrasound correlations. 4th ed. Philadelphia: Elsevier; 2020. p. 327-367.
3. Goodmurphy C, Chiodo A, Haig A: The accuracy of needle placement in extremity muscles: a blinded study. J Clin Neurophysiol 2007;24:366-378.


6. Ryou CH, Shin SY, Kim N, Kim KH, Kim DH, Lee HJ: Safe approach for flexor digitorum profundus I and II using the palmaris longus tendon. Arch Phys Med Rehabil 2022;103:488-493.


7. Chu-Andrews J, Johnson RJ: Electrodiagnosis: an anatomical and clinical approach. Philadelphia: J.B. Lippincott Company; 1986. p. 444.
8. Lee HJ, DeLisa JA: Manual of nerve conduction study and surface anatomy for needle electromyography. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
9. Perotto AO: Anatomical guide for the electromyographer: the limbs and trunk. 5th ed. Springfield: Charles C. Thomas; 2011.
10. American Association of Electrodiagnostic Medicine: Guidelines in electrodiagnostic medicine. Risks in electrodiagnostic medicine. Muscle Nerve Suppl 1999;8:S53-S69.