Electrophysiological and Ultrasonographic Evaluation of Palmar Digital Nerve Injury in Distal Finger
Article information
Abstract
Electrophysiological evaluation of distal lesions in the palmar digital branch of the median nerve presents a significant challenge. We present a case of lateral palmar digital neuropathy of the median nerve, which was confirmed through clinical, electrophysiological, and ultrasonographic assessments. A 54-year-old woman was referred to our electrophysiology laboratory for persistent numbness and a tingling sensation on the radial side of the distal phalanx of her left second finger. She had a laceration injury on the middle phalanx of the second finger and underwent neurorrhaphy of the lateral branch of the palmar digital nerve 8 months ago. Sensory nerve conduction studies, both antidromic and orthodromic, showed low amplitude responses for the lateral branch of the palmar digital nerve. Ultrasonography revealed swelling of this nerve branch within the middle phalanx of the second finger. When patients report sensory symptoms in a specific area, it is important to evaluate for potential cutaneous nerve injuries using electrophysiological studies. Additionally, high-resolution ultrasonography is a valuable tool for investigating small cutaneous nerve lesions, even in the distal finger.
Introduction
The palmar digital branches of the median nerve are responsible for sensation in specific areas of the hand, including the fingers. Mechanical causes, post-traumatic damage, or space-occupying lesions are common causes of neuropathies affecting these branches [1]. Due to their diminutive size and variable pathways, diagnosing injuries to these branches—particularly in the distal finger—can be challenging. Recent advancements have improved the accuracy and efficiency of diagnosing conditions that affect these branches. Electrodiagnostic techniques, such as web space stimulation and the inching test, have been introduced for assessing the palmar digital nerves [2,3]. Additionally, high-resolution ultrasonography has become an invaluable tool for visualizing injuries to these nerves [4,5]. This report details a case of lateral (radial) palmar digital neuropathy of the median nerve in the middle phalanx of the second finger, diagnosed through clinical evaluation, electrophysiological testing, and ultrasonographic imaging.
Case Report
A 54-year-old woman was evaluated in the electrophysiology laboratory for numbness and tingling in the radial aspect of the distal phalanx of her left second finger. Eight months earlier, she had suffered a laceration to the middle phalanx of the same finger, which required neurorrhaphy of the lateral branch of the palmar digital nerve. She reported no history of systemic diseases known to affect peripheral nerves, such as diabetes mellitus or hypothyroidism. Review of the medical record indicated that motor function in the distal finger was intact, with no signs of circulatory impairment. Sensation in the injured finger, however, was estimated to be only about 10% of that in the corresponding finger on the opposite hand. Physical examination revealed normal sensation throughout the entire upper limb, with the exception of hypesthesia on the lateral aspect of the distal phalanx of the left second finger (Fig. 1A). Muscle strength in all upper and lower extremities was found to be normal, as were the deep tendon reflexes, which were symmetrical.

(A) The shaded area demonstrates the location of decreased sensation. (B) Recording electrodes are located on the lateral side of the distal second finger in an antidromic nerve conduction study.
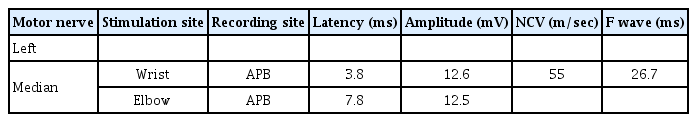
An electrophysiological study of the bilateral upper limbs, including a routine median sensory nerve conduction study (NCS), demonstrated normal responses. The antidromic sensory NCS of the lateral branch of the palmar digital nerve showed a low amplitude of 10 μV. This amplitude was recorded with the active electrode placed at the level of the distal interphalangeal joint and the reference electrode on the fingertip area (Fig. 1B). By contrast, the medial branch of the same finger and the contralateral lateral branch of the second finger exhibited normal amplitudes of 27 and 25 μV, respectively (Tables 1, 2).
As an adjunct to the antidromic sensory NCS, we also conducted an orthodromic sensory NCS of the palmar digital nerve. This involved stimulating the nerve distal to the affected region and placing the recording electrode on the wrist. This approach specifically targets the palmar digital nerve, thereby eliminating potential confounding effects from other nerves. In our study, the patient demonstrated a reduced amplitude of 7 μV upon distal stimulation of the affected area. By contrast, distal stimulation of the contralateral lateral branch yielded an amplitude of 15 μV, which is within the normal range.
Subsequent high-resolution ultrasonography using an 8 to 22 MHz linear probe (RS85; Samsung Medison Co. Ltd., Seoul, Korea) identified a hypoechoic swelling of the left lateral palmar digital branch of the median nerve, located approximately 1 cm distal to the proximal interphalangeal joint in the middle phalanx of the second finger (Fig. 2). The cross-sectional area (CSA) of the swollen nerve measured 3.28 mm2, whereas the CSA of the normal right palmar digital nerve was 0.54 mm2. The patient underwent conservative management, yet some degree of sensory loss persisted in the finger.
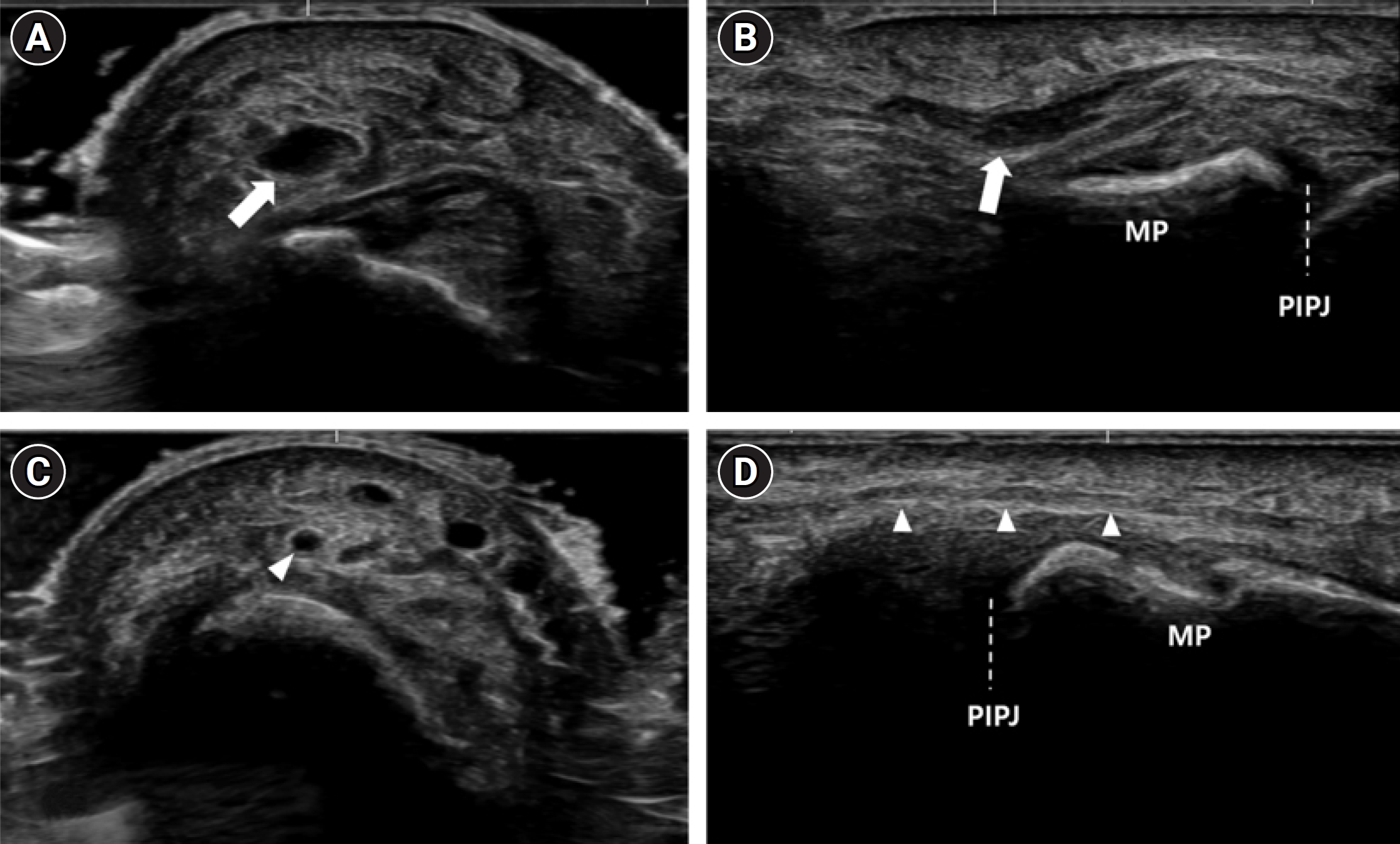
Ultrasonography of the lateral aspect of the second finger middle phalanx (MP) shows a hypoechoic swelling (cross-sectional area [CSA], 3.28 mm2) of the left lateral palmar digital branch of the median nerve (arrows) about 1 cm distal to the proximal interphalangeal joint (PIPJ) in transverse (A) and longitudinal (B) views. The normal right lateral palmar digital branch (arrowheads; CSA, 0.54 mm2) was also demonstrated in transverse (C) and longitudinal (D) views.
The protocol for this report was approved by the Institutional Review Board of our institution (2023AS0202).
Discussion
The patient described in this report presented with numbness and tingling in the lateral aspect of the distal phalanx of the second finger, indicating potential involvement of the lateral palmar digital branch of the median nerve. In a similar case, Noh et al. [6] described a patient who experienced tingling and hypoesthesia in the middle and ring fingers after undergoing a bilateral carpal tunnel release operation. They performed an electrodiagnostic study employing the orthodromic technique, revealing a sensory neuropathy of the palmar digital nerve of the left median nerve.
In this case, electrophysiological studies revealed a lower amplitude in the injured finger compared to the contralateral side and the ulnar branch on the same side, using both antidromic and orthodromic techniques. These results indicate a neuropathic condition affecting the lateral palmar digital branch of the median nerve. Additionally, the sensory nerve action potential (SNAP) amplitude from the antidromic study was higher than that from the orthodromic study, as noted in reference [7]. Consequently, we advocate for the use of the antidromic approach in sensory NCS when assessing cutaneous neuropathy of the finger, if feasible. Nonetheless, employing both antidromic and orthodromic methods yielded thorough and substantial data, enabling a more accurate evaluation of the nerve lesion. This highlights the significance and utility of comprehensive electrophysiologic studies in the investigation of sensory symptoms in targeted areas, which may indicate underlying cutaneous nerve damage.
When a sensory nerve injury occurs in the distal finger, as in this case, positioning the recording electrodes on the target nerve for an antidromic study can be challenging due to the limited space available for recording. To address this, obtaining the SNAP may be facilitated by either narrowing the gap between the active and reference electrodes or by using smaller recording electrodes. For accurate comparison, it is essential to maintain the same distance between the recording electrodes when examining the contralateral side. Caution is also required to ensure that the recording electrode does not inadvertently cover adjacent nerve branches.
As ultrasonography technology has advanced, it has become easier to visualize small cutaneous nerves, although the observer's experience can influence the results [8]. In the case at hand, high-resolution ultrasonography revealed swelling in the lateral branch of the palmar digital nerve. Ultrasonography easily detected even a small, normal palmar digital branch with a CSA of less than 1 mm2. This finding not only corroborated the electrodiagnostic results but also underscored the utility of ultrasonography in diagnosing conditions that affect these diminutive nerves, as evidenced by previous research [4,5]. To the best of our knowledge, despite significant progress in imaging technology, diagnostic imaging has not been routinely employed to assess nerve regeneration following surgical repair [9]. A review of functional magnetic resonance neurography showed thickening of the peripheral nerve at the site of neurorrhaphy [10]. Consequently, we anticipate that ultrasonographic observations post-neurorrhaphy will similarly reveal nerve thickening.
In conclusion, when palmar digital neuropathy in the finger is suspected, a multimodal diagnostic approach that includes electrophysiologic evaluation and high-resolution ultrasonography proves to be useful. For accurate sensory NCS, it is crucial to position the recording electrode precisely over the specific nerve under investigation. This finding contributes to the expanding evidence that highlights the need to consider cutaneous nerve injury in patients with localized sensory symptoms. It also reinforces the value of high-resolution ultrasonography for assessing small cutaneous nerve lesions in the distal regions of the finger.
Notes
Conflict of Interest
Ki Hoon Kim is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts.