Lumbar Plexopathy Due to a Gunshot Wound without Direct Trauma
Article information
Abstract
Lumbar plexopathy resulting from gunshot wounds is rare and is typically associated with open or penetrating injuries. We report a case of lumbar plexopathy caused by a gunshot wound without direct trauma to the plexus. A 77-year-old woman visited the emergency room with a gunshot wound incurred accidentally by a hunter. The entry wound was located on the right lower back, with the exit wound on the left upper arm. The projectiles remained lodged in the paraspinal muscles and had not traversed the fractured vertebral body. Following an emergent left lower pulmonary lobectomy, the patient reported paresthesia and a tingling sensation on the lateral aspects of both thighs. Electrophysiological studies indicated bilateral upper lumbar plexopathy with direct injury to the paraspinal muscles. A low-velocity shotgun injury can transform into high-energy trauma due to the direct impacts of the projectiles, secondary shock waves, and cavitation effects. When neurologic symptoms manifest along a specific dermatome in the lower extremities after a gunshot wound to the lower back, clinicians should consider the possibility of plexopathy, even in the absence of direct trauma to the plexus.
Introduction
The global incidence of gunshot injuries is on the rise along with escalating violence; however, such injuries remain highly uncommon in Korea due to legal restrictions. Moreover, lumbosacral plexopathy resulting from gunshot wounds is particularly rare. This is because traumatic lumbosacral plexopathy is typically linked to fractures of the pelvic or hip joint, which are caused by high-velocity and high-energy trauma, such as falls or motor vehicle collisions [1]. Traumatic lumbosacral plexopathy that does arise from gunshot wounds is associated with open and penetrating injuries [2]. The severity of the damage depends on various mechanical factors of the firearm, including the projectile’s velocity, size, and kinetic energy. Most civilian firearms are characterized by low-velocity and low-energy. In contrast, military and hunting firearms, with projectile speeds exceeding 2,000 to 3,000 feet per second, are considered high-velocity weapons and can inflict severe tissue damage [3]. Injuries from high-velocity weapons can be extensive, and the resulting nerve damage can range from mild conduction block to complete axonal disruption. This report presents the case of a patient who developed lumbar plexopathy due to a gunshot wound, without direct penetrating trauma to the plexus.
Case Report
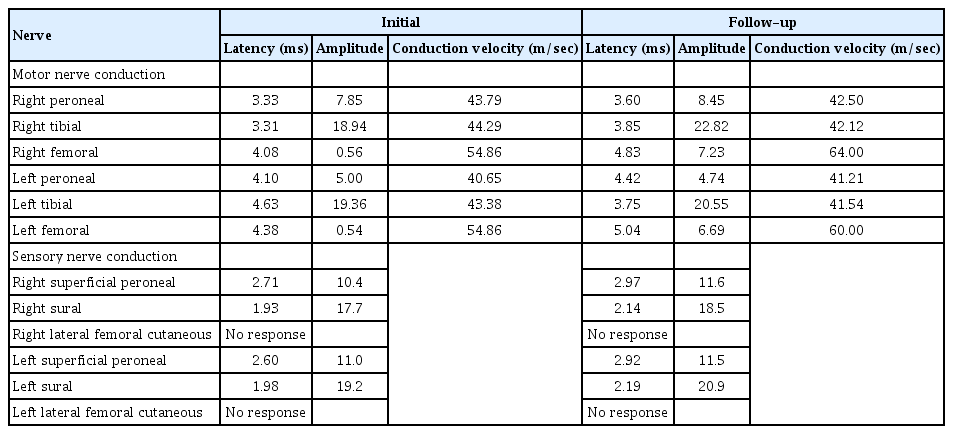
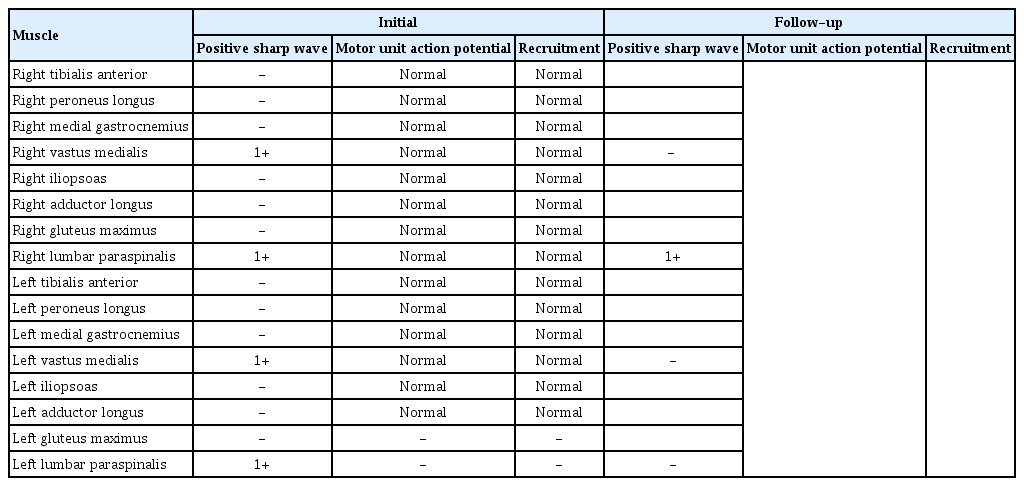
A 77-year-old woman visited the emergency room with a gunshot wound to her lower back, sustained when a hunter mistook her for an animal in the mountains and shot her with a shotgun. The entry wound was located on the right lower back, with the exit wound on the left upper arm. She reported severe pain in her lower back, chest, and left arm. Chest computed tomography revealed metallic hyperdensities in the left lung, lower flank, and back, spanning the left T9–T11 levels and the T12–L3 levels on both sides (Fig. 1). Additionally, multiple fractures were identified in the left 7th–12th ribs, the transverse processes of the left T10–T12 and both L1 and L2 vertebrae, and the spinous processes of the T12 and L1 vertebrae. The projectiles did not traverse the fractured vertebral bodies or the peritoneal cavity, instead lodging in the paraspinal muscles and superficial tissues of the left lower flank. Due to a severe penetrating lung injury, the patient underwent emergent left lower pulmonary lobectomy. Approximately 2 weeks after surgery, the patient reported paresthesia and a tingling sensation in both thighs along the L2–3 sensory dermatome. She displayed no motor weakness, and her deep tendon reflexes were normal. Laboratory tests showed a mildly elevated C-reactive protein level, but other results fell within normal limits. Electrophysiological studies indicated reduced amplitudes of the compound muscle action potentials for both femoral nerves. Sensory nerve conduction studies showed no responses from the bilateral lateral femoral cutaneous nerves (Table 1), and somatosensory evoked potential studies revealed prolonged latencies in these nerves (Table 2). Needle electromyography indicated denervation of both vastus medialis and both lumbar paraspinal muscles at the L2–L4 levels (Table 3). The extensive damage to the back muscles made it challenging to determine whether the denervation potentials in the paraspinal muscles were due to radiculopathy or direct muscle injury. However, the abnormal findings of the nerve conduction studies supported a diagnosis of upper lumbar plexopathy rather than lumbar radiculopathy. These findings were consistent with bilateral upper lumbar plexopathy, accompanied by direct muscle injury to the paraspinal muscles. Magnetic resonance imaging (MRI) of the thoracolumbar spine showed a diffuse bulging disc with left foraminal stenosis at the L5–S1 level (Fig. 2). Pelvic MRI was considered to rule out direct nerve injury by micro-pellets, but the patient declined due to financial limitations.

Chest computed tomography illustrated the trajectory of the shotgun shell, spanning from the right lower back to the left lung and left upper arm.
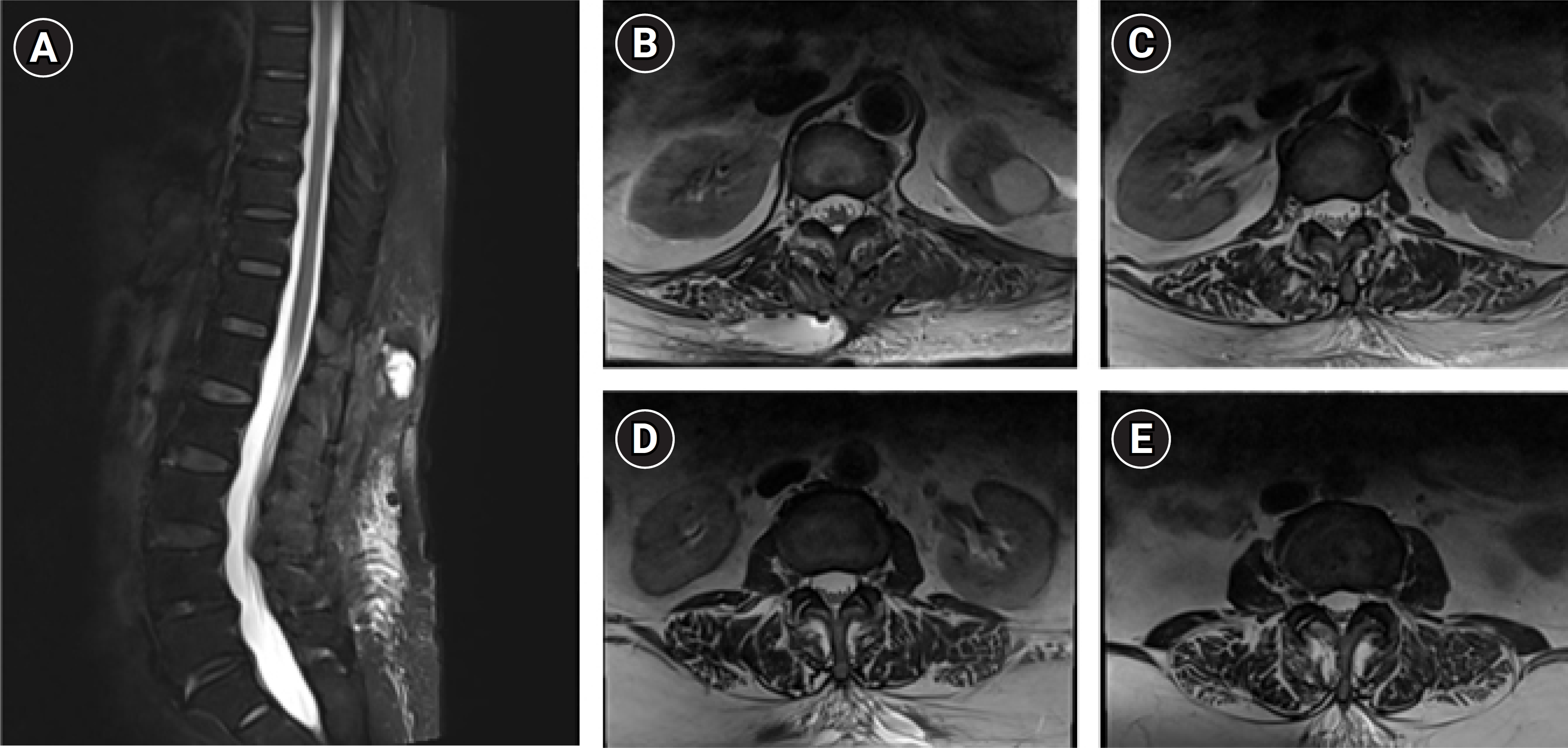
Magnetic resonance imaging of the thoracolumbar spine revealed an intact spinal cord with no signs of neural tissue compression. Sagittal view (A). Axial view at the level of the T12–L1 vertebrae (B), L1–L2 vertebrae (C), L2–L3 vertebrae (D), and L3–L4 vertebrae (E).
The patient’s pain gradually improved with the application of physical modalities and a change in medication from gabapentin to pregabalin. Three months later, follow-up nerve conduction studies and needle electromyography were performed. The lateral femoral cutaneous nerve displayed no interval change, but the amplitudes of the compound muscle action potentials of both femoral nerves had improved to the normal range (Table 1). Needle electromyography no longer revealed denervation potentials in the bilateral vastus medialis and the left lumbar paraspinal muscles, constituting evidence of regeneration (Table 3). These findings suggest the absence of severe axonal loss, with the injury predominantly affecting the sensory branches. This explains the patient’s sensory-dominant symptoms and the probable recovery of motor function within 2 weeks of the injury.
Discussion
This article describes a patient who developed lumbar plexopathy following a shotgun injury. The lumbosacral plexus originates from the anterior rami of the T12–S1 nerve roots and is divided into two parts: the upper lumbar plexus and the lower lumbosacral plexus. The upper lumbar plexus stems from the anterior rami of the L1–L4 roots. As it traverses the psoas muscle, the upper lumbar plexus separates into anterior and posterior branches. The femoral nerve is the principal branch of the posterior division, while the lateral femoral cutaneous nerve, which provides sensation to the anterolateral thigh, also arises from this division [4,5]. In the present case, lumbar plexopathy was localized to the posterior upper quadrant of the lumbar plexus. This observation aligns with findings of a prior study, which indicated that the upper lumbar plexus is more susceptible to injury from gunshots than from motor vehicle accidents, positing that the pelvic brim may shield the lower plexus from gunshot wounds [6].
Due to the bony structure of the pelvis, traumatic lumbosacral plexopathy is less common than brachial plexus injury, although it can be induced by strong impacts such as penetrating trauma or high-velocity injuries [1,2,5]. However, in this case, no penetrating or direct trauma to the plexus was observed.
By convention, firearms that discharge ammunition at velocities exceeding 2,000 to 3,000 feet per second are categorized as high-velocity weapons, while those with muzzle velocities below 1,000 to 2,000 feet per second are classified as low-velocity weapons. Military assault rifles are examples of high-velocity weapons, whereas shotguns and handguns are considered low-velocity weapons. Generally, high-velocity weapons inflict more severe wounds than their low-velocity counterparts [7]. However, the efficiency of energy transfer is as crucial as velocity in determining the extent of damage, which depends on various factors such as the distance to the target and the characteristics of the bullet. As a result, the combination of numerous pellets and a high efficiency of energy transfer at close range renders the shotgun a high-energy weapon. High-energy projectiles can cause nerve damage through several mechanisms, including direct impact, secondary shock waves, and cavitation [8,9]. When a bullet strikes its target, it creates a temporary cavity at the entry point due to traction forces and the vacuum formed by its trajectory. The size and internal pressure of this cavity correlate with the energy transferred by the projectile [8]. With high-energy projectiles, this temporary cavity often yields considerable damage [7,8]. The traction forces and compression from these shockwaves and cavitation are primarily responsible for indirect damage [9]. A previous report documented neurological symptoms following gunshot injury to the spine without direct trauma or penetration of the spinal canal [10]. Similarly, those authors posited that the neural injury in the spinal cord was due to the kinetic energy released by the bullet. Unlike our case, the prognosis in that report was poor. A critical distinction is that, although the bullet did not directly contact the neural tissue in this prior case, imaging examinations revealed its proximity to the neural structures. This underscores the importance of not only the projectile velocity but also the proximity to neural tissue as key determinants.
We report a case of lumbosacral plexopathy occurring without direct trauma to the plexus following a gunshot wound, which is a very rare injury mechanism in Korea. Typically, traumatic lumbosacral plexopathy is associated with clear signs of direct trauma or conspicuous fractures. In the absence of such indicators, delayed diagnosis or misdiagnosis may occur. Consequently, when symptoms such as neuropathic pain, sensory disturbances, or muscle weakness are present along a specific dermatome, clinicians should consider the possibility of plexopathy, even when direct trauma to the plexus is not found. An electrophysiological study is essential to accurately locate the plexopathy, determine the extent of nerve damage, predict the prognosis, and develop an appropriate treatment plan.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.