Novel Pathogenic Variant in PIEZO2 in a Korean Patient with Distal Arthrogryposis
Article information
Abstract
Alterations in PIEZO2 can result in distal arthrogryposis, which is characterized by non-progressive contracture in two or more areas of the body prior to birth. Here, we present a 29-year-old man born with multiple joint contractures and cleft palate. He showed short stature, low-set ears, macrotia, hearing impairment, micrognathia, a triangular face, blepharophimosis, deep-set eyes, high arched eyebrows, decreased facial expressions, retrognathia, arachnodactyly, absent phalangeal crease, shortening of the first and fifth toes, short stature, pectus excavatum, epicanthus, bilateral ptosis, and ophthalmoplegia. He also complained of dyspnea and severe kyphoscoliosis. Pulmonary function tests showed a severe restrictive pattern. An electrodiagnostic study did not reveal any neurogenic or myogenic features. Next-generation sequencing revealed a novel de novo heterozygous pathogenic variant in PIEZO2 (c.7251G>T; p.Trp2417Cys). Our study is the first report of a pathogenic variant in PIEZO2 in a Korean patient with distal arthrogryposis.
Introduction
Arthrogryposis multiplex congenita is a term for inherited disorders that present non-progressive contracture in two or more areas of the body prior to birth. It may occur due to chromosomal disorders, single gene disorders, connective tissue disorders, intrinsic muscle disorders, or abnormalities associated with developmental problem of the central and/or peripheral nervous system [1], and it usually involves arm and/or leg joint contractures [1]. It is a congenital condition that can be accompanied by many other conditions including cleft palate, scoliosis, short stature, and joint contractures [1]. Arthrogryposis multiplex congenita is classified into amyoplasia, distal arthrogryposis (DA), and central nervous system or progressive neurological etiology [1]. DA is a subgroup of arthrogryposis multiplex congenita characterized by non-progressive contractures of the distal regions of the hands and feet without primary neurological or muscular disorders. Currently, 10 different types of DA have been clinically classified, and eight causative genes have been identified [1,2]. The symptom presentation of DA varies widely among patients with the same causative gene, even within a single family with the same variant [3]. Among them, alterations in PIEZO2 can result in DA type 3, DA type 5, DA with impaired proprioception and touch, and Marden–Walker syndrome (MWS) [4-6]. Pathogenic variants in PIEZO2 have been rarely reported in Korea. Herein, we present a novel likely pathogenic variant in PIEZO2 in a Korean patient with DA.
Case Report
A 29-year-old man presented with multiple joint deformities and short stature at an outpatient clinic. He was born at 40 weeks of gestation weighing 2.5 kg to healthy parents, and he displayed multiple joint contractures, particularly in hands and feet (Fig. 1A). He underwent Achilles tenotomy and posterior capsulotomy for the correction of equinus deformity. Surgical procedures to treat cleft lip and palate were also performed. He complained of dyspnea and severe kyphoscoliosis (Fig. 2A). Pulmonary function tests showed a severe restrictive pattern. At 22 years of age, he underwent corrective surgery and began using overnight non-invasive positive-pressure ventilation. At 29 years of age, a physical examination showed multiple contractures of the fingers (including mild camptodactyly), wrists, elbows, toes, ankles, and knees. He exhibited low-set ears, macrotia, hearing impairment, micrognathia, a triangular face, blepharophimosis, deep-set eyes, high arched eyebrows, decreased facial expressions, retrognathia, arachnodactyly (Fig. 2B), absent phalangeal crease, shortening of the first and fifth toes, short stature, pectus excavatum (Fig. 2C), epicanthus, bilateral ptosis, and ophthalmoplegia (Fig. 2D). His touch perception and proprioceptive functions were normal. He did not show ataxia in the extremities or trunk. Although it was difficult to accurately assess motor function owing to the severe joint contractures, there was no definite muscle weakness within the range of motion. Motor function did not change during the 7-year follow-up period. His intellectual function was not impaired. A nerve conduction study showed an amplitude reduction in compound muscle action potential in the lower extremities. Needle electromyography did not reveal any neurogenic or myogenic features. His serum creatine kinase level was 136 U/L (reference range, 55 to 170). These clinical features were compatible with DA. To identify the genetic cause, we performed targeted sequencing of 599 neuromuscular genes (Supplementary Table 1). We identified a heterozygous variant in PIEZO2 (NM_022068.4: c.7251G>T; NP_071351.2: p.Trp2417Cys) (Fig. 1B). The intrafamilial segregation analysis showed that this is a de novo variant.
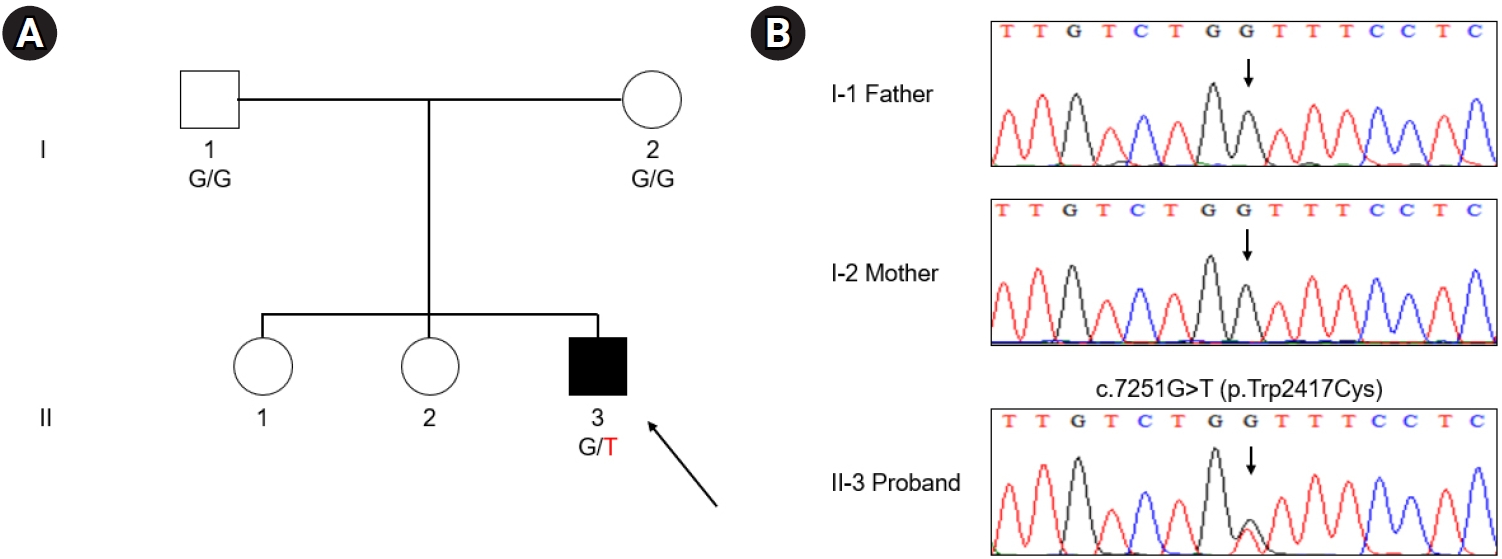
Pedigree, sequencing chromatogram, and clinical features. (A) Pedigree of a patient with distal arthrogryposis. Arrow indicates the proband (square: male; circle: female; filled: affected; unfilled: unaffected). (B) Sequencing chromatograms of the c.7251G>T variant in PIEZO2. The arrow indicates the pathogenic variant site.

Clinical features of a patient with a novel de novo heterozygous variant in PIEZO2. (A) Whole-spine X-ray image. (B) Arachnodactyly. (C) Pectus excavatum. (D) The nine cardinal positions of the gaze.
This report was approved for an Institutional Review Board (IRB) exemption by the IRB of the Gangnam Severance hospital (IRB file number 3-2022-0001). The IRB exemption includes a waiver of the need to obtain signed informed consent.
Discussion
In the present study, we identified a likely pathogenic variant in PIEZO2 in a patient with DA. To the best of our knowledge, this variant has not yet been reported. However, it was classified as a likely pathogenic variant according to the 2015 American College of Medical Genetics and Genomics and the Association for Molecular Pathology guidelines because of the following this evidence: (1) de novo occurrence in a patient (maternity and paternity confirmed) with the disease and no family history; (2) absence from the Genome Aggregation Database full exome and genome databases; (3) multiple lines of computational evidence supporting a deleterious effect on the gene (PolyPhen-2 score: 0.999; SIFT score: 0); and (4) a highly specific phenotype for a disease with a single genetic etiology.
There are 10 types of DA (types 1, 2A, 2B, 3, 4, 5, 6, 7, 8, 9, and 10) (Table 1) [1,2]. Patients must meet two or more major diagnostic criteria of DA to be clinically diagnosed. However, when a first-degree family member is clinically diagnosed with DA, other family members only need one major criterion for a clinical diagnosis [1]. The major criteria are camptodactyly or pseudocamptodactyly, hypoplastic and/or absent flexion creases, overriding fingers, ulnar deviation at the wrist, talipes equinovarus, calcaneovalgus deformities, vertical talus, and metatarsus varus [1]. Our patient had two of the major criteria (camptodactyly and absent phalangeal crease). Different DA types share various common features. However, there are some characteristics that represent each DA types. These characteristics are described in Table 1 [1,3]. Because our patient met the diagnostic criteria of DA and had ocular abnormalities, DA type 5 could be considered as the diagnosis based on his phenotype [1]. DA type 5 patients usually show ptosis, oculomotor dysfunction, deep-set eyes, shortening of the first and fifth toes, and restrictive lung failure with multiple joint contractures, as with our patient. DA is not a progressive disorder. Many children who receive treatment generally have a normal life expectancy although it may be altered by heart involvement and some patients might be born with a fatal condition. Treatment focuses on improving quality of life by correcting deformities and strengthening muscles, mainly through surgical correction and rehabilitation [3]. Ventilation support can be used to those who have respiratory difficulties.
Pathogenic variants in PIEZO2 can result in DA type 3, DA type 5, DA with impaired proprioception and touch, and MWS [4-6]. DA with impaired proprioception and touch is inherited in an autosomal recessive manner [6]. Patients with this type of DA have touch and proprioceptive dysfunction, ataxia, hip dysplasia, finger contractures, foot deformities, and scoliosis [7]. Since our patient did not show misperception of touch sensation, proprioceptive dysfunction, or ataxia, the diagnosis of DA with impaired proprioception and touch was unlikely. DA type 3, DA type 5, and MWS show autosomal dominant inheritance. The key clinical findings of DA type 3, DA type 5, and MWS are cleft palate, ophthalmoplegia, and intellectual problems, respectively. They also can exhibit blepharophimosis, camptodactyly, short stature, micrognathia, scoliosis, and deep-set eyes, with multiple joint contractures, and the prevalence of various symptoms can be different between diseases [1-4]. Although DA type 3, DA type 5, and MWS have traditionally been considered separate disorders, they can also be considered as different expressions of the same condition [4].
The piezo proteins are nonselective cation channels gated by mechanical forces that participate in cell mechanotransduction [8]. Mechanotransduction is the pathway through which mechanical forces are translated into biological signals [8]. It is important for sensory perceptions, such as pain, hearing, touch, and proprioception, and it is also important for embryonic development [8]. There are two types of piezo proteins. The piezo1 protein participates in sensing shear stress in blood vessels, and it plays a critical role in the regulation of vascular tone and the proper formation of blood vessels [9]. The PIEZO2 protein, encoded by PIEZO2, is a mechanotransducer that is mainly expressed in dorsal root ganglia and Merkel cells in the skin [4,10]. PIEZO2 signaling regulates morphogenesis and is related to joint extension, lung or thorax expansion, and oculomotor movement [5]. However, further insights into the precise pathophysiology of pathogenic variants in PIEZO2 causing DA are needed.
In conclusion, a novel de novo heterozygous variant in PIEZO2 was identified in a patient with DA; this is the first reported case in Korea.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by a new faculty research seed money grant of Yonsei University College of Medicine for 2020 (6-2020-0127).
Supplementary materials
Further details on supplementary materials are presented online (available at https://doi.org/10.18214/jend.2022.00171).
List of 598 Neuromuscular-Disorders-Related Genes

