하부 천골신경근 증상으로만 발현된 마미총 증후군 환자에서의 음경해면체근반사와 음부신경 체성감각유발전위검사
Bulbocavernosus Reflex and Pudendal Nerve Somatosensory Evoked Potential in a Cauda Equina Syndrome with Only Lower Sacral Nerve Root Symptoms
Article information
Trans Abstract
Cauda equina syndrome (CES) is a neurological condition involving low back pain, radiating pain, sensory loss, motor weakness, bladder dysfunction, and bowel dysfunction. A 37-year-old man was admitted with saddle-type hypesthesia, bladder dysfunction, and bowel dysfunction, but without motor weakness and radiating pain. He was diagnosed with large sequestrated lumbar disc herniation at L5-S1 and underwent decompression surgery. The initial bulbocavernosus reflex (BCR) and pudendal nerve somatosensory evoked potential (PSEP) on postoperative day 10 showed no response. After 1 month, bladder dysfunction and bowel dysfunction improved and saddle-type hypesthesia slightly improved. We also observed improvement in the BCR and PSEP during a follow-up evaluation on postoperative day 35. These results suggest that BCR and PSEP can indicate improvements in clinical symptoms and improved prognoses for CES patients with bladder dysfunction and bowel dysfunction.
Introduction
Cauda equina syndrome (CES) is a rare but serious neurological disease resulting from compression of the cauda equina, which comprises a bundle of nerves below the first lumbar vertebra. Its incidence is approximately 1 in 33,000 to 100,000 [1]. The most common cause of CES is herniation of the intervertebral disc; however, it occurs in only 1% to 3% of patients with a herniated disc [1]. The second most common cause of CES is tumors, followed by infections, spinal stenosis, hematomas, inflammatory causes, and vascular causes [2]. Because the degree of severity and manifestations of CES vary widely, and because no clear diagnostic criteria exist, clinical suspicion of the condition is important. Clinical manifestations include low back pain, radiating pain, lower limb motor weakness, saddle-type hypesthesia, bladder dysfunction, bowel dysfunction, and sexual dysfunction. The severity of CES symptoms is determined based on the presence of sphincter dysfunction, and manifestations vary accordingly. The bulbocavernosus reflex (BCR) and pudendal nerve somatosensory evoked potential (PSEP) are two tools that can be used to objectively assess the functions of the peripheral pudendal nerve and sacral reflex arc. One study found these to be helpful for determining the degree of severity of CES [3]. However, objective instruments to assess outcomes or improvements in symptoms are lacking. We report a rare case of non-typical CES with bladder dysfunction and bowel dysfunction, but without lower limb motor weakness, radiating pain and low back pain. Improvements in clinical symptoms were assessed using BCR and PSEP in this case.
Case Report
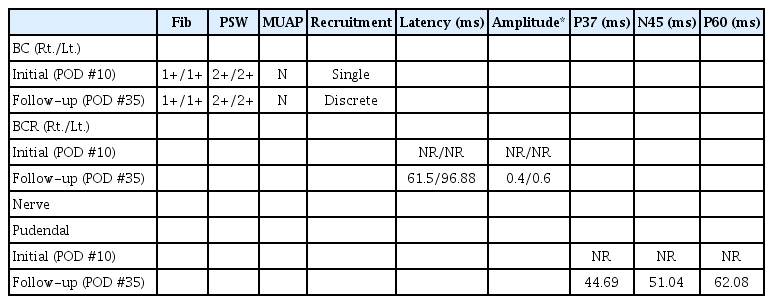
A 37-year-old man had sudden bladder dysfunction, bowel dysfunction and hypesthesia around the anus. He had no notable medical history or trauma, motor weakness, or pain. Lumbosacral magnetic resonance imaging (MRI) performed 1 day after symptom onset showed a sequestrated disc between the fifth lumbar vertebra and the first sacral vertebra inferior migration to infrapedicle level and severely compressed cauda equina nerve roots (Fig. 1A, B). Laminectomy and discectomy were performed 3 days after symptom onset. Although the symptoms did not worsen, bladder and bowel dysfunction persisted after surgery; therefore, he was admitted to the rehabilitative medicine department on postoperative day (POD) 9. At the time of admission, the patient had to use the Valsalva maneuver when urinating. He had a weak urine stream, with 300 to 400 mL of self-voiding and 400 to 500 mL of residual urine. Before symptom onset, he had normal bowel movements once per day; however, after symptom onset, he experienced fecal impaction and incontinence. Physical examination performed at the time of admission showed no abnormal sensory change in the posterior thigh and calf, but perianal hypesthesia in the S3-S5 dermatome. Manual muscle testing revealed normal upper and lower limb muscle strength. The patient had normal patellar tendon and achilles tendon reflex without a pathologic reflex, but he had a weakened BCR. Sensory and motor nerve conduction results for both lower limbs were normal, and both Hoffmann reflexes were in the normal range. During needle electromyography (EMG), all muscles in the lower limbs were normal, but insertion activity and abnormal spontaneous activity were increased in both bulbocavernosus muscles (Table 1). Electrodiagnostic testing of the sacral reflex arc lesions was performed. The BCR and PSEP were absent during the nerve conduction study performed on POD 10 (Table 1). Physical examination results suggested saddle-type hypesthesia and a reduced BCR, and urodynamic test results indicated hyporeflexia of the bladder; therefore, CES was diagnosed. Lumbosacral MRI performed on POD 11 indicated that the cauda equine was no longer compressed (Fig. 1C, D). To control bladder and bowel dysfunction, the patient was administered tamsulosin 0.4 mg, bethanechol 100 mg, and magnesium hydroxide 2,000 mg every day, starting from the day of admission. On POD 35, the patient was able to urinate without using the Valsalva maneuver and did not have the sensation of residual urine; less than 50 mL of residual urine was found after voiding. He regained the ability to have regular bowel movements without fecal incontinence. At that time, delayed BCR latency and normal PSEP were observed. Needle EMG revealed increased insertion activity and abnormal spontaneous activity in both bulbocavernosus muscles (Table 1). Worsening of symptoms was not observed during follow-up, and the patient was able to resume normal daily living.

(A, B) Lumbar spine T2-weighted magnetic resonance imaging shows a sequestrated disc at L5-S1 and severe compression of the cauda equina nerve roots (arrows) in the (A) sagittal view and (B) axial view. (C, D) After bilateral laminectomy and discectomy at L5-S1, the decompressed cauda equina nerve roots (arrows) are observed in the (C) sagittal view and (D) axial view.
Discussion
Although disc herniation is the most common cause of CES, the incidence of CES is low [4,5]. When the cauda equina is compressed, more than 85% of patients experience severe bilateral radiating pain, lower limb weakness, and bladder and/or bowel dysfunction within several hours. However, there have been rare cases of non-typical CES caused by central disc herniation that have involved urinary retention and sphincter dysfunction without radiating pain or lower limb weakness [6].
CES caused by disc herniation may have variable symptoms depending on the location and size of the protruding or sequestered disc. The condition may occur in the upper level (L2-4 nerve roots), middle level (L5-S1 nerve roots), or lower level (S2-5 nerve roots). For example, when the lower level (S2-5 nerve roots) are compressed, saddle-type hypesthesia, decreased anal reflex and BCR, and anal sphincter dysfunction may occur [7]. Anatomically, the lower nerve roots (S2-5 nerve roots) are in a centromedial position in the thecal sac; therefore, central protruding L5-S1 lumbar disc herniation may cause saddle-type hypesthesia, sphincter dysfunction, and decreased anal reflex and BCR without lower limb weakness or radiating pain, as observed in this case.
CES is classified into four stages according to the degree of severity: pre-phase, early-phase, mid-phase, and late–phase. Because sphincter dysfunction such as bladder and bowel dysfunction occur only during the mid-phase and late-phase, the presence of sphincter dysfunction serves as a criterion for determining the severity of CES [3]. However, instruments that enable early diagnosis of CES severity, objective measurements of the prognosis, and determination of improvements in clinical symptoms are lacking. Although physical examination and manual BCR are used as early tools for determining the severity of CES, these have been reported to be unreliable because the results are subjective and vary according to the examiner [8]. Lee et al. [9] reported that BCR and EMG may be useful for predicting the recovery of bladder function in CES patients with bladder dysfunction. Furthermore, BCR and PSEP have been reported to the have the ability to objectively measure the conduction time of the peripheral pudendal nerve and sacral reflex arc, and their latency has been shown to reflect the functions of the peripheral pudendal nerve and sacral reflex arc [10]. Multiple previous studies have used BCR and PSEP to diagnose sexual dysfunction, such as neurogenic erectile dysfunction, but few studies have used BCR and PSEP to diagnose neurologic disorders such as CES [3]. Niu et al. [10] found that BCR and PSEP significantly differed between a normal control group and a peripheral group, including CES patients. Another study reported that BCR and PSEP are helpful not only for diagnosing CES but also for determining the severity of the condition according to the presence of sphincter dysfunction [3]; the results indicated significant differences in BCR and PSEP abnormality rates of CES patients compared to controls, thus confirming that these two parameters have diagnostic value for CES. Furthermore, when CES patients were divided according to the presence or absence of sphincter dysfunction, BCR abnormality rates significantly differed between the two groups.
The patient in the present case had a non-typical case of CES caused by disc herniation that resulted in bladder and sphincter dysfunction, but no lower limb weakness or radiating pain. Therefore, this case highlighted the association between EMG, bladder function, and sphincter function in the absence of other symptoms. The absence of the initial BCR and PSEP response appears to be due to conduction block by nerve compression. The presence of abnormal spontaneous activities such as fibrillation or positive sharp wave indicates that muscle denervation is still in progress. Axonal reinnervation is required for function recovery, but in this case, delayed BCR latency and normal PSEP was observed as clinical symptoms recovered. In the previous study, absent BCR response indicates severe injury of cauda equina, which can lead to a poor outcome of bladder dysfunction of CES [3]. However, the presence of the BCR, either delayed or normal in latency, indicates preserved integrity of sacral arc, which means recovery of bladder dysfunction in CES patients. Therefore, serial follow-up electrodiagnostic study is required.
The patient’s clinical symptoms had further improved at follow-up on POD 45. We expected the EMG results to show corresponding improvements, but the patient refused to undergo an additional EMG due to the discomfort of the test. Although the patient reported sphincter dysfunction, anal sphincter needle EMG could not be performed because he had hemorrhoids and edema at the time. However, we were able to confirm that BCR and PSEP can be indicators of improvements in clinical symptoms for patients with severe CES, bladder dysfunction and bowel dysfunction.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.