 |
 |
- Search
| J Electrodiagn Neuromuscul Dis > Volume 22(1); 2020 > Article |
|
Abstract
Carpal tunnel syndrome (CTS) being the most common entrapment neuropathy makes physicians to easily overlook CTS variants. Here we report two cases of atypical carpal tunnel syndromes which were correctly diagnosed with precise electrodiagnostic findings. One patient seemed moderate to severe degree of CTS at first, but careful electrodiagnostic analysis proved predominant involvement of fascicles of motor nerve and sensory fibers to the thumb, which are located in the radial side of the median nerve. Sonographic findings and MRI demonstrated a mass arising from the median nerve compressing the radial side of the nerve at the wrist. Another patient at a glimpse seemed as mild degree of CTS, but deliberate analysis of electrodiagnostic findings showed separate severe neuropathy of recurrent motor branch of the median nerve. Surgical findings proved these findings and the patient received appropriate surgical treatment, leading to complete resolution of symptoms. Precise analysis of electrodiagnostic findings helped physicians to correctly diagnose these atypical CTS and lead to proper management.
Carpal tunnel syndrome (CTS) is one of the most common entrapment neuropathies.1 Selective fascicular involvement of median nerve or separate injury to the recurrent motor branch (RMB) of median nerve have been reported, but the incidence is rare with less than 1%.2 Due to its rare incidence, physicians are prone to overlook atypical carpal tunnel syndromes and misdiagnose which can lead to mistreatment. Here we report 2 cases of atypical CTS, one of which demonstrated selective fascicular involvement and the other which revealed concomitant RMB neuropathy besides the CTS. Precise electrodiagnostic study was able to distinguish these atypical CTS and lead to appropriate treatment.
A 64-year old female presented with 3-month history of left hand tingling sensation. She has worked in a restaurant for more than 20 years and has overused her hands for dishwashing and chores. The symptom started gradually, with a remote onset of 10 years but quickly aggravated 3 months before her visit. On physical examination, Medical Research Council (MRC) grades of left thumb abduction was grade 2/5 whereas the other muscles were normal. She complained hypoesthesia from her thumb to the middle finger, but the symptom was most severe in her thumb. Left thenar muscle atrophy accompanied. Electrodiagnostic examination was performed in bilateral upper extremities (Table 1). The left median motor response showed prolonged latency and low amplitude (5.1msec, 0.2mV) with abductor pollicis brevis muscle recording. The left “median-second-lumbrical and ulnar-interossei latency comparison study (M2L-PI) revealed negative finding in latency, but the amplitude recorded with second lumbrical muscle was low (3.5msec, 0.1mV with 2L recording; 3.3msec, 6.8mv with PI recording). The left median sensory responses showed prolonged latencies and low amplitudes with the thumb, index and middle finger recordings, but was substantially lower in the thumb (middle finger 11µV, index: 9µV, thumb: 2µV). Needle electromyography (EMG) in the left abductor pollicis brevis (APB) showed abnormal spontaneous activities and polyphasic motor unit potentials with discrete recruitment patterns. This patient was diagnosed moderate to severe degree of left CTS with predominant involvement of fascicles to motor nerve and sensory nerve to the thumb. The patient additionally underwent sonography and magnetic resonance imaging, and a 2x1x8cm mass arising from the median nerve was compressing the volar-radial portion of the nerve (Fig. 1). These findings were compatible with electrodiagnostic findings considering the fascicle distribution of the median nerve, in which the motor nerve and sensory fibers to the thumb is located in the radial side of the median nerve.3,4
A 66-year old female patient presented with 1-month history of right thumb weakness. She had no history of trauma or overuse. MRC scale for right thumb abduction was grade 3/5. She complained no sensory symptoms. Tinel’s sign was equiovocal in the right side. Electrodiagnostic examination was performed in bilateral upper extremities (Table 2). The right median motor response showed prolonged latency and low amplitude (4.2msec, 2.2mV) with abductor pollicis brevis muscle recording. M2L-PI study revealed positive findings for right CTS but the amplitude ratio between second lumbrical and palmar interossei showed insignificant differences in both sides (right side: 3.9msec, 1.8mV with 2L recording and 2.9msec, 4.9mV with PI recording; left side: 3.5msec, 2.4mV with 2L recording and 3.0msec, 6.7mV with PI recording). The right median sensory response showed low amplitude compared to the left side, but the amplitude itself was within normal range (wrist 24µV, palm 28µV).5 In needle EMG, abnormal spontaneous activities and polyphasic motor unit potentials with reduced recruitment patterns were noted in the APB muscle and polyphasic motor unit potentials with reduced recruitment patterns were noted in the second lumbrical muscle. According to the sensory conduction study and M2L-PI study, the patient was diagnosed as mild degree of right CTS, but additionally the findings suggested severe neuropathy of the right RMB of the median nerve. Sonography was performed on the same day and no swelling of the median nerve was found. Surgical findings revealed RMB trespassing the transverse carpal ligament was being compressed by an aberrant vessel (Fig. 2). The orthopedic surgeon ligated the aberrant vessel and released the fascia compressing the RMB, performed RMB neurolysis. Open carpal tunnel release was additionally performed. After, the patient no more complained of right thumb weakness. If the patient was solely diagnosed as mild degree of CTS and had received no surgical treatment or if the patient received endoscopic surgery instead of open carpal tunnel release, the patient would have not recovered.
Until now, electrophysiologic study remains the gold standard for CTS diagnosis. The median sensory conduction study recorded from digit III is most commonly used since the median sensory conduction study is generally considered more sensitive in diagnosing CTS than motor conduction study.6 Moreover, other comparison studies are additionally conducted to allow a more accurate and detailed diagnosis: median-radial sensory latency difference to the thumb, median-ulnar sensory latency difference to the ring finger, median-ulnar mixed nerve latency difference from palm to wrist and second lumbrical-palmar interossei latency comparison study.6,7 These additional studies help physicians to accurately diagnose CTS variants.
Isolated RMB involvement or selective fascicular involvement of the median nerve is reported but the incidence is rare.8-10 In the first case, a mass arising from the median nerve was compressing the median nerve the most at the radial-volar side. According to Planitzer et al., the majority of the motor fascicles of the thenar eminence originates in the radial quadrants and the sensory fascicles of the thumb lies in the radial quadrants, mostly the radial-palmar side.3 Stewart et al has also discovered the fascicular arrangement of the median nerve at the carpal tunnel and found that the motor fascicles are located in the radial-volar side and the sensory fascicles to the thumb are located in the radial side.4 This fascicular structure of the median nerve may cause diverse sensory patterns, which can be misleading to the examiner. The first patient suffered sensory loss in the median nerve innervated territory, the thumb, index and middle finger, but she complained sensory loss in her thumb the most. Also, although her main complaint was sensory symptoms, on physical examination thumb abduction weakness was noted. The electrodiagnostic findings were compatible with the patient’s symptoms and signs: sensory changes especially in the thumb and weakness and atrophy of the thenar muscle.
In the second case, RMB neuropathy was the main problem rather than the mild degree of CTS. In the nerve conduction study, although the M2L-PI study revealed positive results, the amplitude of the second lumbrical was normal. Also, the sensory conduction study revealed low amplitude of the right median response compared to the other side, but the amplitude itself was considered normal.5 To rule out the selective fascicular involvement of the median nerve, sensory nerve conduction study to the index and thumb was additionally done and revealed insignificant results. These findings lead us to make the diagnosis of only mild degree of right CTS, but separate severe neuropathy of the RMB of the median nerve. Surgical findings confirmed RMB trespassing the transverse carpal ligament. There are 3 anatomical courses of RMB of median nerve innervating APB, opponens pollicis, and superficial head of flexor pollicis brevis: extraligamentous, subligamentous and transligamentous courses.8,10 This patient was surgically proven as transligamentous type. The RMB was being compressed by an aberrant vessel and the surrounding fascia. Ligation of the aberrant vessel and releasing fascia, and additional open carpal tunnel release resolved the patient’s motor weakness. If the patient was assumed only mild degree of CTS and had underwent endoscopic surgery or had not received any treatment, the neuropathy might have progressed and eventually lead to poorer prognosis.
Identifying atypical CTS is difficult because the cases are rare and they are unexpected. Through various electrodiagnostic methods, physicians are able to accurately diagnose different types of CTS variants. In these cases, we compared not only the motor and sensory nerve conduction studies, but also sensory nerve recordings in the index and thumb finger and M2L-PI study. Through correct diagnosis, proper management could be made, leading to a favorable outcome.
Fig. 1.
The median nerve (arrowhead, A) is being compressed by a mass arising from the median nerve, especially in the radial-volar side of the nerve (arrow, B, C) (D=dorsal, V=volar, R=radial, U=ulnar).
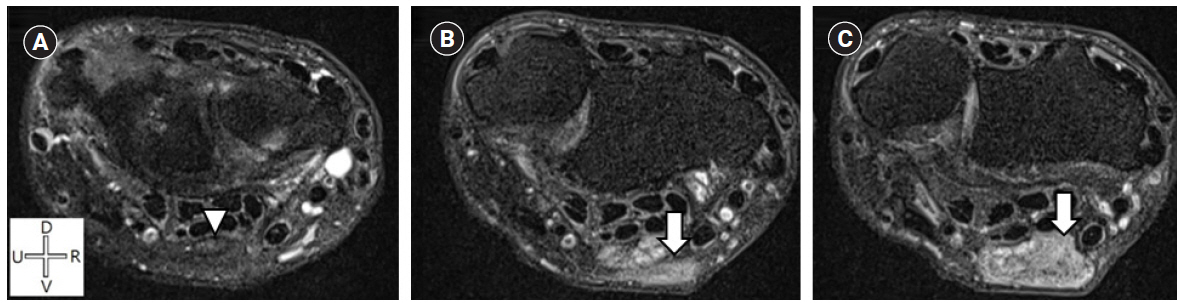
Fig. 2.
Surgical findings of Case 2 confirmed RMB (arrow) trespassing the transverse carpal ligament being compressed by an aberrant vessel (arrowhead).
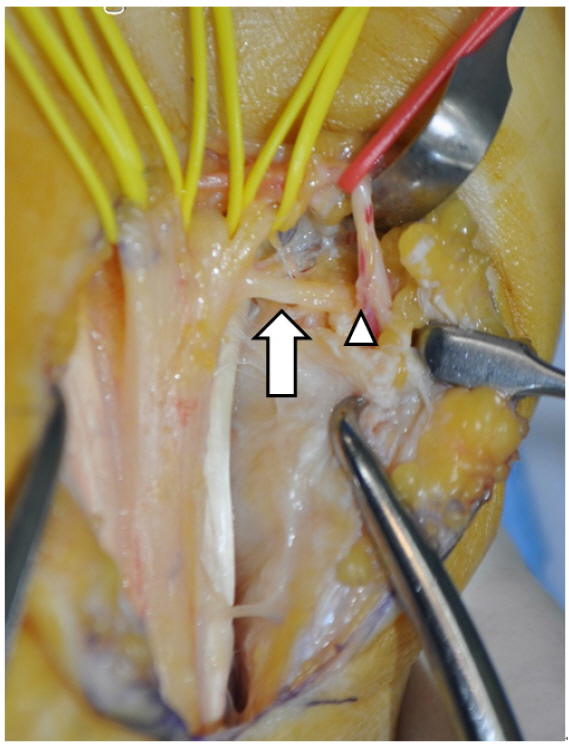
Table 1.
Motor and Sensory Nerve Conduction Study of Case 1
| Motor nerve conduction | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Side | Nerve | Stimulation site | Recording site | Latency (msec) | Amplitude (mV) | Distance | NCV (m/sec) | F wave (msec) | |||
| Left | Median | wrist | APB | 5.1* | 0.2* | 18 | 53 | 27.2 | |||
| Ulnar | wrist | ADM | 2.9 | 13.8 | 17 | 65 | 25.5 | ||||
| Left | Median | wrist | 2nd lumbrical | 3.5 | 0.1* | ||||||
| Ulnar | wrist | 1st palmar interosseous | 3.3 | 6.8 | |||||||
| Sensory nerve conduction | |||||||||||
| Side | Nerve | Stimulation site | Recording site | Onset/peak latency (msec) | Amplitude (µV) | ||||||
| Left | Median | wrist | III digit | 3.6/4.4* | 11* | 14 | |||||
| palm | III digit | 0.9/1.6 | 20 | 7 | |||||||
| wrist | II digit | 2.9/3.8* | 9* | 14 | |||||||
| wrist | I digit | 3.0/4.2* | 2* | 10 | |||||||
| Ulnar | wrist | V digit | 2.8/3.6 | 24 | 14 | ||||||
Table 2.
Motor and Sensory Nerve Conduction Study of Case 2
| Motor nerve conduction | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Side | Nerve | Stimulation site | Recording site | Latency (msec) | Amplitude (mV) | Distance (cm) | NCV (m/sec) | F wave (msec) | |||
| Right | Median | wrist | APB | 4.2 | 2.2* | 17.5 | 58 | 25.2 | |||
| Ulnar | wrist | ADM | 3.3 | 8.2 | 15 | 65 | 23.6 | ||||
| Right | Median | wrist | 2nd lumbrical | 3.9* | 1.8 | ||||||
| Ulnar | wrist | 1st palmar interosseous | 2.9 | 4.9 | |||||||
| Left | Median | wrist | 2nd lumbrical | 3.5 | 2.4 | ||||||
| Ulnar | wrist | 1st palmar interosseous | 3 | 6.7 | |||||||
| Sensory nerve conduction | |||||||||||
| Side | Nerve | Stimulation site | Recording site | Onset/peak latency (msec) | Amplitude (µV) | Distance (cm) | |||||
| Right | Median | wrist | III digit | 2.6/3.3 | 24* | 14 | |||||
| palm | III digit | 1.0/1.8 | 28* | 7 | |||||||
| wrist | II digit | 1.8/2.4 | 31* | 14 | |||||||
| wrist | I digit | 2.4/3.0 | 28* | 10 | |||||||
| Ulnar | wrist | V digit | 2.4/3.2 | 22 | 14 | ||||||
| Left | Median | wrist | III digit | 2.3/3.0 | 45 | 14 | |||||
References
1. Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH: Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve 1993;16:1392-1414.

2. Rizzello G, Longo UG, Franceschi F, Martinelli N, Meloni MC, Quadrini R, et al: Compression neuropathy of the motor fibers of the median nerve at wrist level. J Chin Med Assoc 2009;72:268-270.


3. Planitzer U, Steinke H, Meixensberger J, Bechmann I, Hammer N, Winkler D: Median nerve fascicular anatomy as a basis for distal neural prostheses. Ann Anat 2014;196:144-149.


4. Stewart JD: Peripheral nerve fascicles: anatomy and clinical relevance. Muscle Nerve 2003;28:525-541.


5. Chen S, Andary M, Buschbacher R, Del Toro D, Smith B, So Y, et al: Electrodiagnostic reference values for upper and lower limb nerve conduction studies in adult populations. Muscle Nerve 2016;54:371-377.


6. Lee HJ, Kwon HK, Kim DH, Pyun SB: Nerve conduction studies of median motor nerve and median sensory branches according to the severity of carpal tunnel syndrome. Ann Rehabil Med 2013;37:254-262.




7. Lee S, Kim D, Cho HM, Nam HS, Park DS: Diagnostic Value of the Second Lumbrical-Interosseous Distal Motor Latency Comparison Test in Severe Carpal Tunnel Syndrome. Ann Rehabil Med 2016;40:50-55.




8. Bennett JB, Crouch CC: Compression syndrome of the recurrent motor branch of the median nerve. J Hand Surg Am 1982;7:407-409.








