내측 팔꿈치에 발생한 결절종에 의한 양측성 주관절터널증후군 증례
A Case of Bilateral Cubital Tunnel Syndrome Associated with Ganglion Cysts in Medial Elbow
Article information
Trans Abstract
Here, we report a patient with bilateral cubital tunnel syndrome caused by both medial elbow ganglion cysts. The patient complained of paresthesia in the ring and small finger with weakness in both the hands caused by the gradual enlargement of a soft mass that was felt in both medial elbows for about three years. The patient complained of difficulty in using chopsticks and bringing the fingers together. Electrodiagnostic study revealed bilateral ulnar neuropathy at elbow level. Suspecting a ganglion cyst, an ultrasound and magnetic resonance imaging studies were performed. Aspiration of these cysts (a yellow jelly-like fluid) had improved patient’s symptom and electrodiagnostic findings in follow-up study. It is rare that a medial elbow ganglion leads to ulnar neuropathy. We report a case where the patient’s symptoms improved with conservative treatment without surgical excision.
Introduction
Cubital tunnel syndrome is the second most common compressive peripheral neuropathy occurring in the upper limbs.1 There are five areas in all where the ulnar nerve can be compressed. Among them, the cubital tunnel has the most frequent incidence of compression (arcade of Struthers, the medial intermuscular septum, the medial epicondyle, the cubital tunnel, and the deep flexor pronator aponeurosis).1 A ganglion cyst is a tumor-like lesion of unknown origin, which is surrounded by compact connective tissues filled with gelatinous fluid.2 Symptomatic ganglion cysts are common in wrist and knee, however, medial elbow ganglion cysts are also infrequently reported.3 Ganglion cysts may cause compressive peripheral neuropathy at several sites.3 Of the total cases exhibiting cubital tunnel syndrome, those caused by a medial elbow ganglion cyst account for only 8% of the cases.3 Although, compressive ulnar neuropathy by a medial elbow ganglion cyst has been reported, bilateral ganglion cyst compression of the ulnar nerve occurring in the cubital tunnel is not reported.1,3 Here, we report a case of bilateral cubital tunnel syndrome caused by medial elbow ganglion cysts in bilateral elbows observed in a 62-year-old male patient, which showed improvement with mass aspiration alone without surgical treatment.
Case report
A 62-year-old male patient with a history of diabetes was visited to the outpatient clinic complaining of gradual deterioration of senses and weakness in both hands that had lasted since the last 2 years. The patient noticed a mass on the medial side of both elbows 3 years ago. He complained of pain (visual analog scale, VAS: Right, 10; Left,9) and paresthesia in the ring finger, small finger, and medial palm of both the hands which started 2 years ago. In addition to atrophies of hypothenar muscle and first dorsal interosseous muscle, he complained of weakness that made it difficult for him to use chopsticks. He also complained of tingling sense in both 1st to 4th finger. The patient had a history of diabetes but no history of injury to the elbows or hands. He ran a restaurant where it is inevitable to use his elbows and hands in order to cook meat. His mother and brother had similar symptoms with mass development on both elbows, and these masses were aspirated with a syringe.
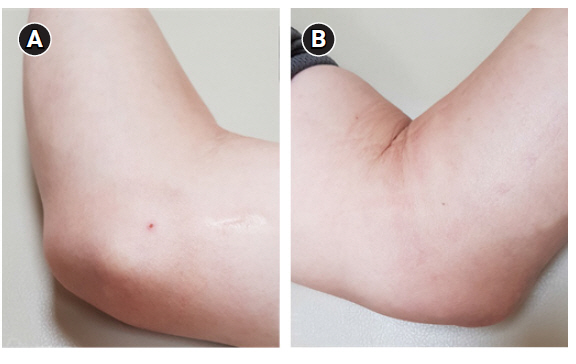
Palpable masses were observed from the nuchal area and both elbows medially (Fig. 1). There was no tenderness around the masses. Neurological examination revealed paresthesia in the ring finger, small finger, and the medial area of the palm in both the hands. The grasping power had been weakened to Grade 4 in both hands and mild atrophy was observed in the intrinsic and hypothenar muscles. However, wrist flexion power was normal in both the hands. Claw hand or Froment sign was not observed, but Wartenberg’s sign was observed in both the hands. The Tinel sign was positive at both the elbows. There was no sensory abnormality in the lower extremities and the deep tendon reflexes of both upper and lower extremities were normoactive.
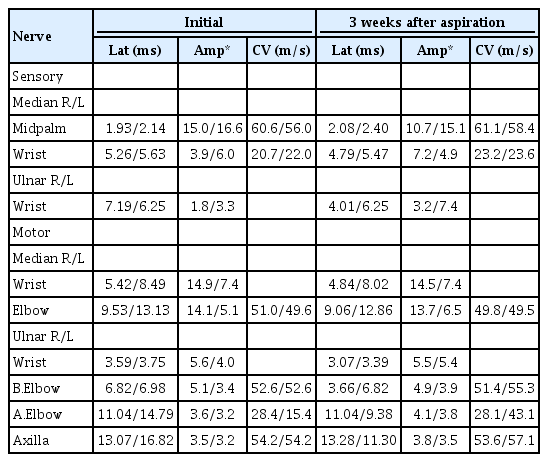
In the nerve conduction study (NCS), the peak latency of sensory nerve action potentials (SNAPs) were delayed in the both median and ulnar nerves with decreased amplitude. In the compound muscle action potentials (CMAPs) of the both median and ulnar nerves, a decrease in velocity was observed in the wrist and elbow area, respectively (Table 1). Needle electromyography (EMG) showed abnormal spontaneous activity in the abductor digiti minimi (ADM) and the first dorsal interosseous muscle from both sides and a decreased recruitment pattern. In flexor carpi ulnaris, however, EMG findings were normal. Based on the NCS and EMG results, median neuropathies and ulnar neuropathies were confirmed at the wrists and elbows, respectively. Since a hypoechoic mass was observed along the ulnar nerve at both the elbows in the ultrasound study (Fig. 2), magnetic resonance imaging (MRI) was conducted for more accurate diagnosis. MRI of the right elbow showed a lobulated extraneural mass with a maximal size of 1.3 * 2.9 * 3.8 cm, which was observed up to the cubital tunnel, with compression of the ulnar nerve (Fig. 2). This was indicative of an ulnar neuropathy caused by a ganglion cyst.

(A/B) Ultrasound images of both medial elbows. (A) right elbow, (B) left elbow. (C/D) T2-weighted MRI images of right elbow showed compressed ulnar nerve by surrounded cysts. Arrows mean ulnar nerve. (C) coronal view, (D) axial view.
To release the compression, percutaneous aspirations were done around the masses from both sides using a 22-gauge needle with ultrasound induction. 2 cc and 3 cc of the fluid were removed from the right and left side respectively. These generated a yellowish jelly-like fluid from both the masses (Fig. 3). The mass was almost invisible to the naked eye from the left side after aspiration. The mass was still visible to the naked eye from the right side; however, further aspiration was not possible. Cytopathological examination conducted on the aspirated product revealed no malignancy.
The patient revisited our outpatient clinic 3 weeks after the aspiration and the size of mass had not increased. Pain and paresthesia from both hands still remained but their intensity had decreased. The paresthesia was partially improved in the both hands. The pain showed improvement from VAS 10 to 4 in the right hand and VAS 9 to 3 in the left hand. The left hand showed greater improvement in general and the intensity of the Tinel sign also decreased. However, there was no clear motor recovery. In the follow-up analysis of nerve conduction study, the delay of peak latency from the SNAP decreased and the amplitude increased in the right ulnar nerve. The peak latency from the SNAP was the same on the left side but the amplitude increased. CMAP amplitude did not show a significant difference in the right ulnar nerve, but the conduction velocity increased in the section the elbow from the CMAP of the left ulnar nerve (Table 1).
Discussion
Cubital tunnel syndrome is a second-most common peripheral neuropathy of the upper limbs following carpal tunnel syndrome. Cubital tunnel syndrome can be caused by the mechanical or dynamic compression of the ulnar nerve and has various symptoms.4,5 Cubital tunnel syndrome associated with medial elbow ganglion cyst has been rarely reported. Although the origin of a ganglion cyst is controversial, it has a strong association with osteoarthritis.4 According to a case series regarding the compression of the ulnar nerves, a ganglion cyst originates entirely from the medial side of the ulnohumeral joint.4 Ganglion cysts are either bilobular or multilobular and cubital tunnel syndrome caused by a ganglion cyst shows rapid deterioration. Therefore, ultrasound or MRI images are crucial for determining the location of the compressed nerves.4,6
Ganglions causing peripheral neuropathy are intraneural or extraneural cysts.7 Intraneural ganglions are mucinous cysts that develop within epineurium of nerves.8 Extraneural ganglions are common mucinous cysts outside of the epineurium of peripheral nerve.8 The extraneural cysts are connected to joints through capsule tears which is located separate from an articular branch.8 To treat the intraneural ganglions, articular branch ligation and nerve decompression were recommended.1 Treatment of extraneural cysts is total resection.1 Surgical treatment was more effective than conservative managements such as aspiration, intralesional steroid injection, sclerotherapy, hyaluronidase, and threat technique.9 However, conservative managements had fewer complications, which can be used to relieve symptoms if the patient deos not want surgery.9 Aspiration alone method is one of conservative managements and the simplest to management ganglion cyst.9
In our case, ganglionic cysts which caused bilateral ulnar neuropathy were treated with percutaneous aspirations. Recurrence of mass was not observed for 3 weeks after the aspiration and there was also no clinical deterioration. In addition to improvement in symptoms, the results of NCS showed an increase of the left CMAP velocity around the elbow joint. This indicates that the compression caused by the mass was partially released as a result of aspiration. The symptoms remained as the cyst could not be aspirated fully, but the patient’s discomfort was largely resolved.
We report a case of bilateral cubital tunnel syndrome caused by ganglion cysts in both elbows that have not been reported. The primary treatment for cysts is surgical excision. However, we demonstrate here that aspiration of the medial elbow ganglion cyst alone can be effective as a conservative treatment. Further follow-ups are warranted to clarify long term prognosis of conservative treatment.