무지구근 운동분지의 완전 전도차단을 보이는 정중신경병증
Complete Conduction Block of the Thenar Motor Branch
Article information
Trans Abstract
Thenar motor neuropathy is a rare, pure motor neuropathy of the median nerve with delayed motor latency in electrophysiological studies. We present an extremely rare case of idiopathic thenar motor neuropathy with complete median motor conduction block at the carpal tunnel level, which was confirmed by ultrasonographic and surgical findings. Right median nerve conduction studies demonstrated normal sensory responses and no motor response in the abductor pollicis brevis (APB). Needle electromyography of the right APB showed no recruitment of motor unit action potentials. Ultrasonographic examination demonstrated enlarged and swollen median nerve fascicles within the carpal tunnel. A carpal tunnel release operation was performed; the median nerve underneath the transverse carpal ligament was swollen and blanched due to decreased vascularity, suggesting the presence of compression. Pain in the thenar area improved 2 weeks after surgery. Herein, we emphasize the usefulness of ultrasonographic evaluations in determining the level of the nerve injury in cases with doubtful electrophysiological results.
INTRODUCTION
Thenar motor neuropathy (TMN) is a rare disorder presenting as a motor neuropathy involving the thenar muscles without sensory disturbance, and is commonly confirmed by electrophysiological studies. In most previously reported cases of TMN, the level of the median nerve injury was evident from the results of electrophysiological studies, or the causative lesion, such as iatrogenic injury, trauma, or presence of compressive mass, was obvious.1–3 However, in case of idiopathic TMN with the complete conduction block on nerve conduction study (NCS), ultrasonographic evaluation may be the key to identifying the cause of TMN. Herein, we describe a rare case of TMN due to median nerve compression at the level of the carpal tunnel, which was confirmed by electrophysiological, ultrasonographic, and surgical findings.
CASE REPORT
This study was approved by the Institutional Review Board and the requirement for informed consents were waived.
Patient History and Physical Examination
A 56-year-old woman presented with pain and weakness in the thenar area of the dominant right hand. The symptoms started 1 month earlier without any history of trauma. She was working as a surveyor and handled repetitive manual paperwork. Clinical examination revealed severe paresis of right thumb abduction and opposition with no visible contraction of the thenar muscle. On manual muscle examination, the patient’s right finger flexors, wrist volar flexor, and wrist dorsiflexor were normal. There was no atrophy of the right thenar muscles or other intrinsic hand muscles; the right hand showed no hypoesthesia. Phalen’s test was positive in the right wrist.
NCS
The right median motor NCSs showed no motor response in the right abductor pollicis brevis (APB). Median motor NCSs at the pronator quadratus showed no abnormal findings bilaterally. The second lumbrical/dorsal interossei technique, a sensitive test for carpal tunnel syndrome (CTS), was performed; there was no significant difference in the median and ulnar nerve latencies (Table 1). Results of motor NCSs of the bilateral ulnar nerves and orthodromic sensory NCSs of the bilateral median, ulnar, and radial nerves were normal. The median and ulnar sensory latencies recorded on the 4th finger were not significantly different (Table 2). Skin temperature measured during the study was > 32℃.
Needle Electromyography
Needle electromyography of the right APB showed no evidence of abnormal spontaneous activities at rest and no recruitment of motor unit action potentials during volition. There were no abnormal findings in the flexor carpi radialis and the flexor pollicis longus, which are innervated by the median nerve and the anterior interosseous branch, respectively. No abnormal findings were observed in the muscles innervated by the C8-T1 roots, namely, the first dorsal interosseous, abductor digiti minimi, and extensor indicis proprius. Because the patient had pain in the thenar area, the muscles innervated by the C5-6 roots were also evaluated; there were no abnormal findings in the biceps brachii and deltoid muscles.
Ultrasonography
Ultrasonographic evaluation was performed using the GE LOGIQ P6 Pro (General Electric, Milwaukee, WI, USA) with a 3.42–10.85-MHz linear probe. No direct compressing mass-like lesion was observed around the right median nerve and the recurrent motor branch (RMB). Compared to the left, the right median nerve, proximal to the carpal tunnel (cross-sectional area, 13.60 vs. 7.17 mm2) and within the carpal tunnel (cross-sectional area: 11.45 vs. 7.89 mm2), was enlarged. The median nerve fascicles within the carpal tunnel showed significantly lower echogenicity on the radial side. On ultrasonographic examination, the RMB was observed to originate from the radial side of the median nerve and passed extraligamentously. RMB thickness was 0.60 mm in the right and 0.52 mm in the left side (Fig. 1). There was no evidence of thenar muscle atrophy
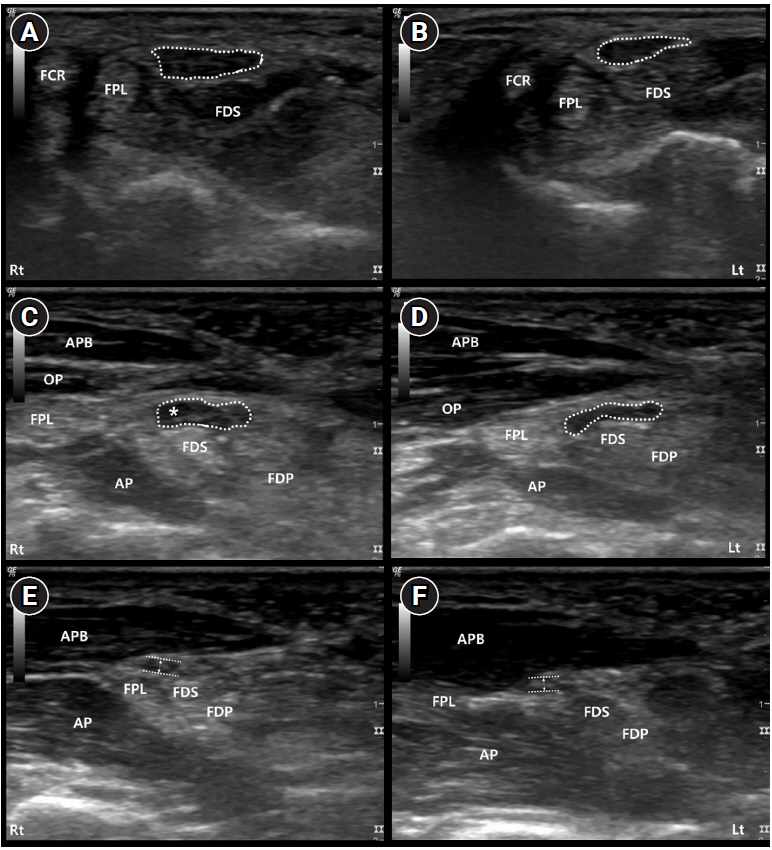
Ultrasonographic findings of the median nerve. The median nerve (dotted) is enlarged at the proximal carpal tunnel level in the right (A) as compared to the left (B). Swollen radial side motor fascicles (asterisk) within the median nerve are observed on the right side in the distal carpal tunnel (C, D). Recurrent motor branch originates from the median nerve distal to the transverse carpal ligament (extraligamentous course) in the right (C) and left (D) sides without the presence of compressive lesion in the right (E) or left (F) sides.
APB, abductor pollicis brevis; AP, adductor pollicis; FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus; OP, opponens pollicis.
Surgery
The symptoms showed no relief despite therapeutic administration of injectables from the local clinic and prescription of oral medication for a month; therefore, surgical treatment was decided. An extended carpal tunnel release operation of the right hand was performed. Intraoperatively, the median nerve underneath the transverse carpal ligament appeared blanched (due to decreased vascularity) and swollen proximally, suggesting the presence of a compressive lesion at the carpal tunnel (Fig. 2). The RMB (arrow) had an extraligamentous course after branching from the main median nerve, with no definite swelling or presence of adjacent tumorous lesion. The thenar area pain improved 2 weeks after surgery. A follow-up electrophysiological evaluation was scheduled 3 months after the surgery, but the patient refused further follow-up because the pain had subsided.
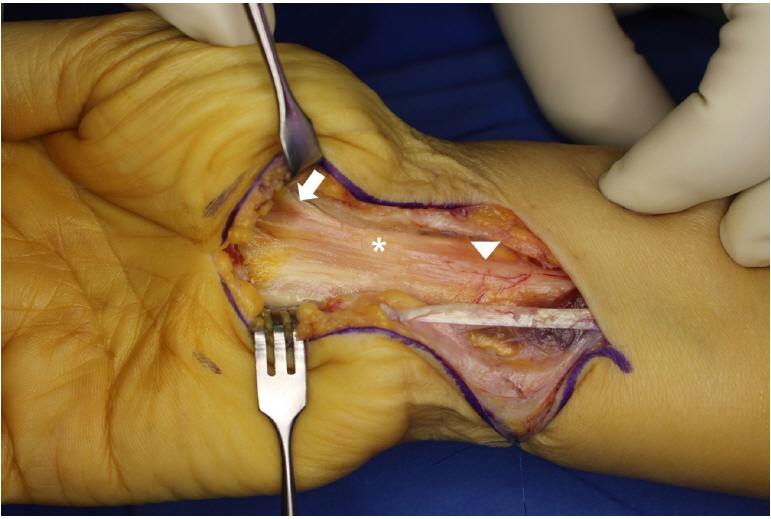
An incision was made across the wrist crease and the flexor retinaculum was retracted to expose the median nerve (arrowhead). The median nerve underneath the transverse carpal ligament (asterisk) was blanched due to decreased vascularity, suggesting the presence of a compressive lesion. The recurrent motor branch (arrow) had an extraligamentous course after branching from the main median nerve, with no definite swelling or surrounding tumorous lesion.
DISCUSSION
CTS is reportedly the most common entrapment neuropathy. Sensory symptoms predominate in early CTS. As the disease progresses, there are continuous and severe sensory symptoms in combination with motor symptoms. Sensory fibers are more vulnerable to early nerve injuries and are usually affected first and more severely than motor fibers.
TMN is an isolated compression of the motor fibers and characterized by weakness of the median nerve-innervated thenar muscles without sensory disturbance. TMN is extremely rare and accounts for only 1.2% of all median neuropathies of the wrist.4 It is diagnosed by electrophysiological examination, and shows prolonged distal motor latency and normal sensory conduction velocities.1
In our case, sensory NCSs were normal, but there was no thenar muscle response on motor NCSs. We stimulated the median nerve at the wrist and recorded the response in the 2nd lumbrical muscle; the response was normal. These findings are contrary to that observed in typical CTS, and can be explained by complete conduction block of the median motor fibers to the thenar muscles. However, it was difficult to determine whether TMN occurred from the median nerve or the RMB only with the result of NCS.
TMN is usually considered as an isolated neuropathy of the RMB caused by direct traumatic or iatrogenic damage2; space-occupying masses, such as ganglion cysts3; or isolated compression of the RMB.1 Besides definitive nerve injury, some author have proposed that occupational activities could influence the incidence of TMN. In previous studies, the prevalence rate of TMN was higher in the Korean population,5 vineyard workers, and Brazilian hand-milkers.6 These higher prevalence in specific populations indicated that the occupations and lifestyles, such as repetitive manual work, cause minimal but chronic direct trauma, which leads to TMN.
Anatomical variations in the course and branching of the median nerve have been reported, and extraligamentous course of the RMB is the most frequent anatomical variation.7-8 Subligamentous or transligamentous course could be potential risk factors for isolated compression of the RMB.1 Moreover, previous studies have reported that motor fascicles oriented in the extreme radial side of the median nerve in most cases (60%), and consequentially, the RMB was frequently observed to originate on the radial aspect.9 In our case, there was no evidence of alterations in the RMB; moreover, the median nerve was swollen and blanched, suggesting a compressive lesion at the carpal tunnel. Thus, our case was presumptively diagnosed as idiopathic TMN at the median nerve due to CTS.
Ultrasonographic evaluation may be the key to identifying the obscure cause of TMN. Pathological information, such as ganglion cyst and schwannoma, can be assessed using ultrasonography. Ultrasonography is a reliable tool for diagnosing CTS, with cut-offs for median nerve cross-sectional areas ranging from 8.5–10 mm.2,10 Ultrasonography can also indicate the characteristics of RMB, such as severely thickened RMB or its anatomical course.8 In our case, ultrasonography showed an extraligamentous course of RMB without thickening or surrounding compressing mass. Median nerve swelling on the radial side was identified, which corresponded to the previous finding of anteroradially-located thenar motor fascicles in the median nerve.3,8,9 Since most previous cases of TMN occurred at the level of RMB, evident from the findings of NCS or etiology, our unusual case of idiopathic TMN at the carpal tunnel level and its diagnostic process are noteworthy.
Our study had the following limitations. First, stimulation at the palm in the median motor study, recorded at the APB, need to be conducted to confirm the level of nerve injury. Second, although the right thenar pain subsided 2 weeks after surgery, we could not evaluate the patient using electrophysiological and ultrasonographic studies postoperatively.
Delayed distal latency in the motor nerve conduction study of the median nerve with normal sensory response is the key finding to diagnose idiopathic TMN. In the absence of motor response with normal sensory stimuli, diagnosis of TMN is challenging and ultrasonographic evaluation of the median nerve and the RMB is useful to assess the presence, location, and cause of nerve compression. We suggest the combined use of electrophysiological study and ultrasonography for the diagnostic evaluation of TMN with complete motor conduction block.


