 |
 |
- Search
| J Electrodiagn Neuromuscul Dis > Volume 22(1); 2020 > Article |
|
Abstract
Objective
To determine the role of somatosensory evoked potential (SEP) study for axillary nerve and confirm clinical usefulness through case studies.
Method
Fifteen healthy volunteers were recruited for the axillary nerve SEP study. The stimulation site is located on the posterior edge of the lateral deltoid muscle. The active recording electrode is placed over the contralateral C3' or C4' scalp area. Fz was used as the reference. The latency and amplitude of axillary nerve SEP were estimated. SEP data was compared by gender and correlation with height and age was also analyzed. Two patients diagnosed with axillary nerve injury through a nerve conduction study were collected for the axillary nerve SEP.
Results
In healthy subjects, N1 latency was 13.8Âą0.9 msec, and P1 latency was 20.1Âą1.8 msec. The amplitude was 1.35Âą0.53 ăś. The average amplitude difference between right and left sides was 0.26Âą0.20 uV. In patients with axillary nerve injury, the axillary nerve SEP was found to be absent or significantly reduced in amplitude. Female subjects showed larger amplitudes and shorter N1 and P1 latencies than male subjects. There was no significant correlation between height and SEP data.
Conclusion
It is meaningful that our study is the first study to make the normal value of axillary nerve SEP and apply it to patients with axillary nerve injury. The axillary nerve SEP study may be helpful for patients with axillary nerve injury who have discomfort in the shoulder or impaired sensation on the lateral side of the upper arm.
The axillary nerve arises from the posterior cord and lies on the side of the radial nerve and proceeds behind the shoulder joint. Then the nerve passes through the quadrilateral space and moves around the posterior and lateral sides of the proximal humerus. A muscular branch is given off to the teres minor muscle. The axillary nerve ends in two muscular branches, anterior and posterior, and innervates the deltoid muscle. An upper lateral cutaneous nerve of the arm arises from the posterior branch of axillary nerve. This nerve provides cutaneous sensation to the region of skin overlying the deltoid muscle.1
Most evaluation of the axillary nerve are limited to motor conduction studies. There have been few studies of sensory nerves in the axillary nerve. Because the sensory nerve action potential of axillary nerve is little known.1 Somatosensory evoked potential (SEP) studies, as well as nerve conduction studies, can help diagnose peripheral neuropathy.1-4 Clinical use of peripheral nerve SEP is increasing because monitoring of SEP of peripheral nerves during limb surgery such as limb lengthening and deformity correction is popular.5
If it is possible to pick up the SEP study for axillary nerve, it will help you evaluate the pure injury of sensory branch of axillary nerve. Therefore, this study was performed to determine the role of axillary nerve SEP and to confirm its clinical usefulness through a case study.
In this study, 15 healthy volunteers (8 males and 7 females) without a history of stroke, spinal cord injury, or peripheral neuropathy were recruited to measure the normal value of axillary nerve SEP. The mean age of the subjects was 28.1Âą3.5 years (27.8 males, 28.6 females, range 24-38 years). The average height was 168.7Âą7.9 cm (174.5 males, 162.0 females, range 157.0-180.0 cm). All subjects were described and agreed to the study and the IRB approved the study.
For the potential analysis, an electromyography recording system, DantecTM KEYPOINTÂŽ (Alpine Biomed Aps, Skovlunde, Denmark) was used. The active recording electrode is placed over the contralateral C3â or C4â scalp area. Fz was used as a reference recording site. In a preliminary study, C1â/C2â and C3â/C4â were compared as active recording sites. According to the neuroanatomical location, C1â/C2â was expected to be superior to C3â/C4â because the shoulder sensory cortical area is medial to hand sensory cortical area. However, in this study, we were able to find the largest amplitude when using C3â/C4â as the active recording sbibrite. A stimulus duration of 0.2 msec is used at 3.2 Hz. Bandwidth was 3 Hz - 3 KHz. Anatomically, the sensory branch of the axillary nerve is behind the deltoid muscle. The stimulation site is localized on the posterior edge of the lateral deltoid muscle (Fig. 1). The stimulus intensity was adjusted to about 2-3 times the sensory threshold, and could produce a visible twitch in the deltoid muscle. Negative peak latency, positive peak latency and peak to peak (N1-P1) amplitude of axillary nerve SEP were estimated. SEP waves were averaged with 300 stimuli, and two waves were acquired on each side of the arm.
After measuring the control value of the axillary nerve SEP, it was applied to patients diagnosed with axillary neuropathy through a nerve conduction study.
SPSS 16.0 software was used for statistical analysis. Parametric t tests were analyzed to find the difference between latency and amplitude in both sides of axillary SEP study in healthy controls. The Mann-Whitney test between gender and SEP data was analyzed. The non-parametric correlations were analyzed to evaluate the relationship between height and SEP data. The results were found to be statistically significant at pďź0.05.
In healthy subjects, the N1 latency was 13.8Âą0.9 msec, and the P1 latency was 20.1Âą1.8 msec. Peak to peak amplitude (N1-P1) was 1.35Âą0.53 ăś. The difference in amplitude was not statistically significant on the right and left sides (Table 1).
In axillary SEP latency and amplitude by gender in healthy controls, female subjects appeared to have larger amplitudes and shorter N1 and P1 latencies than male subjects. It was statistically significant (p<0.05) (Table 2).
In axillary SEP latency and amplitude according to the height of the healthy control group, the height showed a positive correlation with N1 and P1 latency in right side, N1 latency in left side, but it showed a negative correlation with amplitude in both sides. It was statistically significantly (p<0.05) (Table 3). There was no significant relation between age and SEP data. The Spearman non-parametric correlation coefficient study analyzed the correlation between age and SEP data, such as N1, P1 latency, or peak-to-peak amplitude, and all correlations were not significant (Table 3).
Two patients with axillary nerve injury showed abnormalities in the axillary nerve SEP study (Figs. 2, 3). One patient did not show the evoked potential in axillary nerve SEP on the lesion side, so a complete axillary nerve palsy was suggested. (Fig. 2). Other patient showed a decrease in amplitude on the lesion side, thus suggesting partial axillary nerve palsy (Fig. 3).
Case 1: A 14-year-old boy visited the clinic with pain and weakness in his right shoulder. Four months ago, his right shoulder hit a lurching bus. After trauma, weakness in the right shoulder and numbness around the deltoid muscle occurred. In an MRC manual muscle test in upper limb, he showed zero in right shoulder abduction. In nerve conduction studies, the right axillary nerve compound muscle action potential was not evoked, but other examined nerves were within normal limit. In needle electromyography, teres minor and deltoid muscles innervated by axillary nerve were completely denervated, but all examined muscles innervated by other nerves were normal. He was diagnosed with complete peripheral neuropathy of right axillary nerve. In the axillary SEP study, it did not show any remarkable potential in right axillary nerve stimulation, Nl latency 13.6 msec, P1 latency 20.9 msec, and the amplitude 0.83 uV in left side (Fig. 2).
Case 2: A 73-year-old woman was transferred to Department of Rehabilitation Medicine after a surgery for the humeral neck facture. Two months ago, she slipped and injured, and after the operation, pain and weakness in the left shoulder occurred. In an MRC manual muscle test in upper extremity, he showed 3 in left shoulder abduction. The sensory around the deltoid muscle have been reduced. In the motor nerve conduction study, the latency was within normal limit in both axillary nerves, but the left axillary nerve compound muscle action potential amplitude was halved compared to the right. In the needle electromyography, there was a finding of partial denervation potential in the deltoid muscle on the lesion side. She was diagnosed with partial peripheral neuropathy of the left axillary nerve with a nerve conduction study and electromyography. In the axillary nerve SEP study, Nl latency 14.6 msec, P1 latency 19.7 msec, amplitude 1.18 uV on the right, Nl latency 15.0 msec, P1 latency 22.2 msec, amplitude 0.67 uV on the left side. The N1-P1 amplitude decreased on the left (Fig. 3).
The majority of closed axillary nerve injury occurs in association with a glenohumeral dislocation and/or fracture of the surgical neck of the humerus.6 Trauma due to blunt damage directly to the nerves has also been reported, also. When the patient visits the clinic with such a medical history, the clinician should propose axillary nerve injury, and conduct an electrodiagnostic evaluation to differentiate the axillary nerve injury from other neuropathies. Axillary nerve lesions are the most common, but posterior cord level of brachial plexopathy can develop.7 Sometimes, the patient may have separated the motor branch injury of the axillary nerve.8 In addition, some athletes with axillary nerve injury or suprascapular nerve injury may have asymptomatic even if complete or incomplete lesions persist.9
Pain is not a prominent complaint, and deltoid weakness is often masked by compensation from surrounding muscle groups.10
Uncommonly but, there is a pure sensory neuropathy in axillary nerve, such as sharp cutting injury by knife to the lateral arm. In such a case, conventional nerve conduction study and electromyography will be normal. In this case, axillary nerve SEP can be done for more exact approach of nerve injury. In addition to pure sensory neuropathy, axillary nerve SEP used to identify abnormalities in the central nervous system pathway expected from medial and tibial nerve SEP, and to utilize it in incomplete brachial plexopathy, proximal cervical radiculopathy or other proximal peripheral neuropathies.
The diagnostic value of somatosensory evoked potentials in the diseases of peripheral nervous system is increasing. Especially, in pudendal neuropathy, diabetic neuropathy, and trigeminal neuropathy, SEP study seems to be helpful to assess the degree of peripheral neuropathy.4,11,12
Female subjects showed larger amplitude and shorter latency of axillary nerve SEP than male. Such findings represent in other SEP or sensory nerve conduction study also.13-15 However, it was too narrow age spectrum and small sample size of control group to know the correlation between the age and the latency of axillary SEP. In the further study, the study should be done in more broad range of age.
Limitation of this study was as follows; at first, small sample size, second, a technical difficulty of axillary SEP study arise from relatively short distance between stimulating and recording electrode. However, we expect that the axillary nerve SEP developed in this study will provide more options for diagnosing axillary nerve injury. Axillary nerve SEP study would not be an essential method to diagnose axillary neuropathy. But if you consider axillary nerve SEP technique, it will be a helpful method to diagnose axillary nerve injury.
It is meaningful that this study was the first study making normal value of axillary nerve SEP and applying it to the patients with axillary nerve injury. Although we couldnât find the patient who experiences just only reduced sense in axillary nerve territory of lateral upper arm, the axillary nerve SEP study might be useful in the patients whose are suggestive of a pure sensory type of axillary neuropathy, brachial plexopathy, proximal cervical radiculopathy, or other proximal peripheral neuropathies. In such case, we could find clinical usefulness and auxiliary role of the axillary SEP study.
Fig. 1.
Stimulation site for sensory branch of axillary nerve: at the posterior margin of the lateral deltoid muscle. (Yellow triangular area).
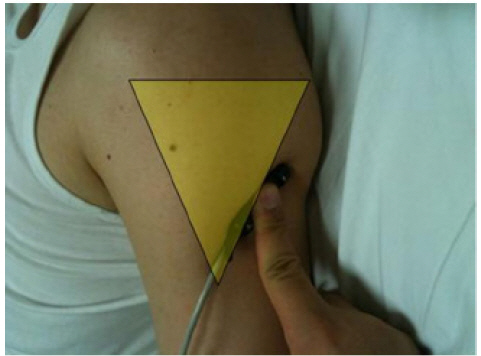
Fig. 2.
Axillary nerve SEP in Case 1. (Fig. 2-A) Sound side, (Fig. 2-B) Affected side. In affected side, there werenât any remarkable waveforms.
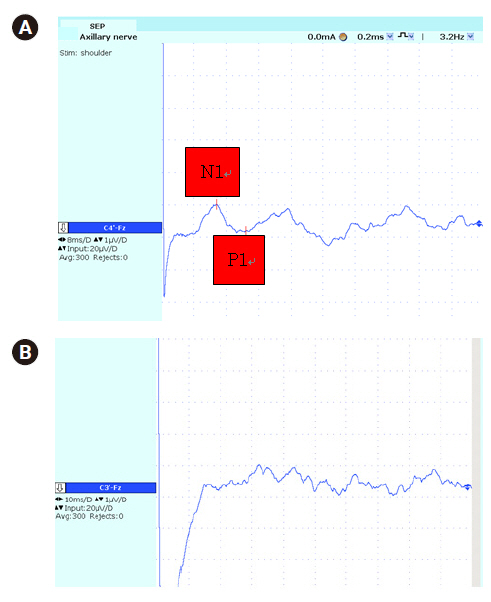
Fig. 3.
Axillary nerve SEP in Case 2. (Fig. 3-A) Affected side, (Fig. 3-B) Sound side. In affected (left) side, N1-P1 amplitude was markedly reduced compared to sound (right) side, but N1 & P1 latency was not significantly different in both sides.
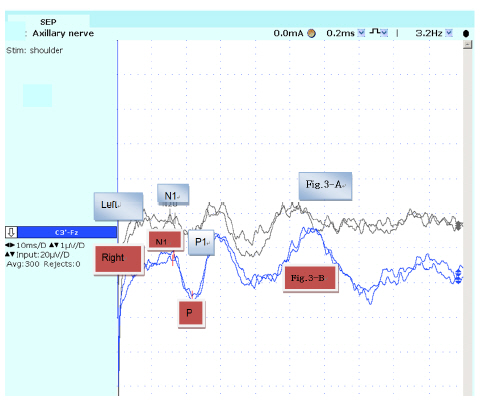
Table 1.
Normal Value of Axillary Nerve Somatosensory Evoked Potential
| N1 Latency (msec) | P1 Latency (msec) | Amplitude (ăś) | L-R amplitude difference |
|---|---|---|---|
| 13.8Âą0.9 | 20.1Âą1.8 | 1.35Âą0.53 | 0.26Âą0.20 |
| (12.6-15.3) | (16.5-22.6) | (0.55-2.60) | (0.04-0.76) |
Table 2.
Amplitude and Latency in Each Gender
| Right | Right | Right Amplitude | Left | Left | Left Amplitude(ăś) | |
|---|---|---|---|---|---|---|
| N1 (msec) | P1 (msec) | (ăś) | N1 (msec) | P1 (msec) | ||
| Male | 14.3Âą0.9 | 21.0Âą1.3 | 1.06Âą0.38 | 14.2Âą0.6 | 21.1Âą1.2 | 1.10Âą0.44 |
| Female | 13.3Âą0.7 | 18.7Âą1.4 | 1.67Âą0.49 | 13.1Âą0.6 | 19.2Âą2.2 | 1.66Âą0.56 |
| p value* | 0.035 | 0.015 | 0.021 | 0.005 | 0.048 | 0.043 |
| Total | 13.8Âą0.9 | 19.9Âą1.8 | 1.35Âą0.52 | 13.7Âą0.8 | 20.2Âą1.9 | 1.36Âą0.56 |
References
1. Dumitru D, Zwarts M: Brachial plexopathies and proximal mononeuropathies. In: Electrodiagnosticn Medicine, 2nd ed, Philadelphia, Hanley & Belfus, 2001: 808.

2. Eisen A, Elieker G: Sensory nerve stimulation and evoked cerebral potentials. Neurol 1980;30:1097-1105.

3. Tsukamoto H, Sonoo M, Shimizu T: Segmental evaluation of the peripheral nerve using tibial nerve SEPs for the diagnosis of CIDP. Clin Neurophysiol 2010;121:77-84.


4. Lee EC, Kim EJ, Park CH, Hong SH, Kim MO: Somatosensory Evoked Potentials from the Three Branches of the Trigeminal Nerve and Clinical Correlation. J Korean Assoc Electrodiagn Med 2016;18:11-17.

5. Makarov MR, Samchukov ML, Birch JG, Cherkashin AM, Sparagana SP, Delgado MR: Somatosensory evoked potential monitoring of peripheral nerves during external fixation for limb lengthening and correction of deformity in children. J Bone Joint Surg Br 2012;94:1421-6.


6. Dumitru D, Newton BY, Dreyfuss P: Segmental vs dermatomal somatosensory evoked potentials: Normal intertribal variation and side-to-side comparison. J Phys Med Rehabil 1993;72:75-83.

7. Liveson J: Nerve lesions associated with shoulder dislocation: an electrodiagnostic study of 11 cases. J Neurol Neurosurg Psychiatry 1984;47:742-744.



8. Kallio MA, Kovala TT, Niemelä EN, Huuskonen UE, Tolonen EU: Shoulder pain and an isolated teres minor nerve lesion. J Clin Neurophysiol 2011;28:524-527.


9. Safran MR: Nerve injury about the shoulder in athletes, part 1: suprascapular nerve and axillary nerve. Am J Sports Med 2004;32:803-819.


10. Alnot JY: Traumatic brachial plexus palsy in the adult. Retroand infraclavicular lesions. Clin Orthop Relat Res 1988;237:9-16.

11. Ărmeci B, AvcÄą E, Kaspar Ă, Terim ĂE, ErdoÄru T, Ăge AE: A Novel Electrophysiological Method in the Diagnosis of Pudendal Neuropathy: Position-related Changes in Pudendal Sensory Evoked Potentials. Urology 2017;99:288.

12. Seyit DA, Degirmenci E, Oguzhanoglu A: Evaluation of Electrophysiological Effects of Melatonin and Alpha Lipoic Acid in Rats with Streptozotocine Induced Diabetic Neuropathy. Exp Clin Endocrinol Diabetes 2016;124:300-6.



13. Bolton CF, Carter KM: Human sensory nerve compound nerve action amplitude: Variation with sex and finger circumference. J Neurol Neurosurg Psychiatry 1980;43:925-928.



14. Stetson DS, Albers JW, Silverstein BA, et al: Effect of age, sex. And anthropometric factors on nerve conduction measures. Muscle Nerve 1992;15:1095-1104.
-
METRICS

-
- 0 Crossref
- Scopus
- 3,359 View
- 75 Download
- Related articles in J Korean Assoc EMG Electrodiagn Med
-
The Determinant for N20 Latency of Somatosensory Evoked Potentials in Infants2019 December;21(2)





