The Hmax/Mmax Ratio as a Diagnostic Tool in Assessing Spasticity in a Patient with Hereditary Spastic Paraplegia
Article information
Abstract
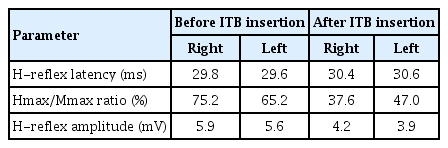
Hereditary spastic paraplegia (HSP) refers to a group of inherited diseases caused by progressive degeneration of the corticospinal tracts. We report a case of an HSP patient with ankle spasticity treated with an intrathecal baclofen (ITB) pump, for whom the Hmax/Mmax ratio was used as a diagnostic tool for spasticity. A man in his early 30s who was born without any complications and developed normally in childhood was diagnosed with HSP when he was 29 years old. Equinus gait pattern and bilateral genu recurvatum improved after manual therapy and botulinum toxin injections in both gastrocnemius muscles; however, after a few months, his gait disturbance became more severe as a natural course of the disease. To treat ankle spasticity and clonus, he was considered a suitable candidate for an ITB therapy. However, as spasticity is a finding that is easy to recognize but difficult to evaluate, we conducted electrophysiological testing, including H-reflex and the ratio of H-reflex amplitude to compound muscle action potential amplitude. The Hmax/Mmax ratio was 75.2% on the right side and 65.2% on the left side before an ITB pump, and 37.6% on the right side and 47.0% on the left side after an ITB pump. This case illustrates the usefulness of testing electrophysiological parameters such as the Hmax/Mmax ratio to measure spasticity objectively in late-onset HSP patients. The Hmax/Mmax ratio is also a good tool for measuring the degree of improvement in spasticity after ITB or additional treatment in these patients.
Introduction
Hereditary spastic paraplegia (HSP) refers to a clinically and genetically heterogeneous group of inherited neurodegenerative and neurodevelopmental disorders caused by progressive degeneration of the corticospinal tracts [1]. Clinically, these conditions manifest as lower limb spasticity, weakness, hyperreflexia, and other corticospinal signs. The genetic basis of HSPs includes mutations inherited through autosomal dominant, autosomal recessive, and X-linked patterns. Its classification is based on the sequential numbering of chromosomal loci or specific genes, as they were identified, using a spastic paraplegia gene (SPG) designation [2]. Currently, more than 70 SPG genes have been described, and yet, since many conditions mimic HSP, accurate diagnosis can be challenging [1].
HSP patients show slow and progressive gait disturbances, as well as spasticity from infancy to adulthood. Currently, there is no specific disease modification therapy for HSP. Symptomatic treatment includes physiotherapy, anti-spasticity drugs (baclofen, tizanidine and diazepam), and botulinum toxin. An orthosis is important for preventing complications, which can include multiple contractions, pain, and fractures, as well as for improving the patient’s quality of life [3,4].
Here, we report a case of an HSP patient with ankle spasticity who was assessed with the Hmax/Mmax ratio and treated with an intrathecal baclofen (ITB) pump. The patient complained of severe ankle spasticity and gait disturbance. Initially, the spasticity of both ankles scored grade 1+ on the modified Ashworth scale (MAS). Despite undergoing rehabilitation therapy and receiving injections, the patient's ankle clonus and spasticity worsened. We decided on an ITB pump after assessing the patient’s spasticity using the Hmax/Mmax ratio. We aim to illustrate the difficulties in the decision of ITB insertion in this HSP patient with spasticity, and to emphasize the importance of using the Hmax/Mmax ratio in making this decision.
Case Report
A male patient in his early 30s, who was born without complications and developed normally during childhood, began to experience ankle spasticity and gait disturbance at the age of 26. These conditions progressively worsened. Despite his conscious efforts to walk normally, he gradually began to trip and drag both feet as if they were not under his control. His walking pattern exhibited pes equinus, genu valgus, and a waddling gait. He was admitted to the neurology department of our hospital, where genetic studies revealed a pathogenic mutation in SPAST gene (MIM 604277), specifically an exon 9-16 duplication. At the age of 29, he was diagnosed with HSP. Brain magnetic resonance imaging demonstrated no definite abnormality.
The patient exhibited grade 3 muscle weakness in both ankle dorsiflexion and plantar flexion, as classified by the Medical Research Council. He was able to walk independently, and his functional independence measure was 123. He scored 53 on the Berg balance test. Both knee and ankle jerks were hypertonic, and ankle clonus was sustained. In terms of spasticity, both ankles’ plantar flexors had MAS scores of 1+. A sensory examination showed hypesthesia on both ankles. Due to ankle spasticity and clonus, he presented to our rehabilitation center and started pool therapy, and circuit training (chest press, rowing, back machine, leg extension, and leg curl) for 2 months. Due to HSP, the patient presented with core muscle weakness, lower limb muscle weakness, and spasticity. We performed manual therapy to relieve his symptoms. Although this treatment helped with his muscle strength and gait disorders, joint contracture, and spasticity, thereby improving the patient’s daily life functions and relieving pain, the discomfort persisted. However, as his spasticity worsened, we administered an initial injection of 300 units of Dysport (Ipsen, Boulogne-Billancourt, France)) was injected first into both gastrocnemius muscles. Six months later, due to continued spasticity, we administered 200 units of Botox (Allergan, Dublin, Ireland) into both gastrocnemius muscles. Following these injections, both the equinus gait pattern and genu recurvatum showed improvement. However, a few months later, the patient's gait disturbance worsened, reflecting the natural progression of the disease.
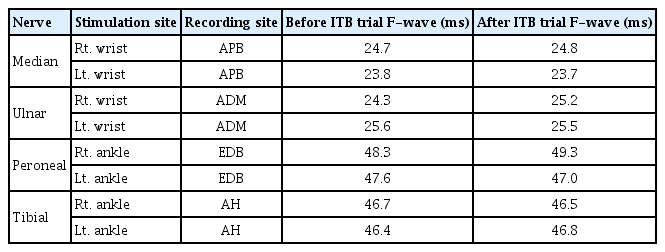
This patient was deemed an appropriate candidate for an ITB therapy, aimed at managing severe ankle spasticity and clonus. However, given that spasticity is a symptom that is easy to identify but challenging to evaluate, we carried out electrophysiological tests, including the H-reflex and the ratio of the H-reflex to that of compound muscle action potential amplitude (Fig. 1). The H-reflex and M-response of the bilateral gastrocnemius–soleus (triceps surae) muscles and the F-wave of the tibial nerve recorded from each abductor hallucis longus muscle were assessed. The patient was positioned supine with a slight knee flex (approximately 30°). The ankle joint was secured in a mild plantar flexion position (around 20°), as the H-wave of the soleus muscle is inhibited by ankle dorsiflexion. The Hmax/Mmax ratio was 75.2% on the right side and 65.2% on the left side, leading us to decide on the use of an ITB pump (Tables 1, 2).

Electrophysiological evaluation of lower motor neuron excitability, H-reflex and M-wave in a patient with hereditary spastic paraplegia. (A) The H-reflex and M-wave forms before intrathecal baclofen pump treatment. (B) The H-reflex and M-wave forms after intrathecal baclofen pump treatment.
No significant side effects were observed following the ITB bolus injection, which led us to proceed with the ITB pump insertion. The infusion dose was initiated at 25 µg/day and was incrementally increased to 60 µg/day. Following the continuous ITB infusion, there was a reduction in ankle spasticity and clonus. The MAS score for both ankles improved with plantar flexor scores from 1+ to 1. Improvements were also noted in both the equinus gait pattern and genu recurvatum. A subsequent study of the Hmax/Mmax ratio showed values of 37.6% on the right side and 47% on the left side (Table 1).
Discussion
One of the primary objectives of rehabilitation is to recover from gait disorders, which significantly hinder functional independence in HSP patients. In our patient, spasticity was particularly evident in both ankles, specifically in the ankle plantar flexors. This patient experienced gait disturbance, and it is important to note that spasticity is one of the most common causes of gait disorders.
The MAS is commonly used to measure spasticity, but it is not sensitive enough to determine small changes in spasticity, and its reliability has been reported to be variable depending on the muscle and joint in question [5]. The MAS is thought to be more reliable among those assessing upper extremity spasticity, but it is not reliable for spasticity in the lower extremities [6,7]. In plantar flexion spasticity, the short-lever arm of the ankle makes it difficult to determine resistance to movement [6,7].
Currently, no treatment regimens for HSP are available. As the disease typically progresses, effective symptomatic treatment can significantly reduce the patient's disease burden. HSP is characterized by the degeneration of the corticospinal tract and dorsal column in a length-dependent manner. This degeneration manifests as key clinical features such as bilateral lower limb spasticity, a positive Babinski sign, and hyperreflexia [8]. ITB can improve spasticity and gait ability in patients with HSP [9]. However, in some cases, like our patient, it may be difficult to assess spasticity precisely with a physical examination. In such cases, electrophysiological parameters (H-reflex and the Hmax/Mmax ratio, and F-wave response) can measure spasticity more objectively and can be used as a part of the clinical evaluation [10]. The Hmax/Mmax ratio is a comparison of the total and maximum counts of motor neurons that are reflexively activated by excitatory and inhibitory stimuli. This ratio decreases in the presence of presynaptic inhibition and reduced motor neuron excitability [11]. Previous studies have found that, compared to healthy individuals, the H-reflex amplitude is significantly higher on the spastic side in patients with spasticity [12,13]. Another study demonstrated that the Hmax/Mmax ratio is a feasible and objective method for quantifying the decrease in motor neuron excitability in patients with cerebral palsy [14]. However, there are notable variations in the Hmax/Mmax ratio among individuals with the same degree of hypertonia, which accounts for the poor correlation [15].
Only one report has utilized the Hmax/Mmax ratio to evaluate spasticity in a patient with HSP [16]. Unlike the other study, our case emphasizes the usefulness of the Hmax/Mmax ratio in a patient with HSP who complained of spasticity and had a MAS score that did not align with that complaint. In our patient, the MAS scores were 1+ in both ankles, and the degree of discomfort expressed by the patient did not match those findings. Thus, it was difficult to decide whether to proceed with ITB insertion. An electrophysiological test was conducted to assess the degree of spasticity via the Hmax/Mmax ratio, which was 75.2% and 65.2% on right and left side, respectively. We decided to insert the ITB pump. After the ITB pump therapy, we assessed the Hmax/Mmax ratio again, and it showed improvement. The Hmax/Mmax ratio accurately measured the patient’s spasticity, enabling rapid ITB pump insertion, which improved the patient’s quality of life.
In conclusion, our HSP patient had spasticity and mild motor weakness. The symptoms began in adulthood and progressed slowly and steadily; therefore, it was not easy to assess spasticity in a precise manner. The MAS score and degree of spasticity experienced by the patient did not match. In such a case, it may be useful to test electrophysiological parameters, such as the Hmax/Mmax ratio, to measure spasticity objectively. Furthermore, the Hmax/Mmax ratio is a good measure to estimate the degree of improvement in spasticity after ITB insertion or other treatments in HSP patients.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.