 |
 |
- Search
| J Electrodiagn Neuromuscul Dis > Volume 25(2); 2023 > Article |
|
Abstract
Granular cell tumors, also known as Abrikossoff’s tumors, are rare soft-tissue tumors, and their occurrence in the peripheral nerves has been very rarely reported. We present the case of a 35-year-old woman with common peroneal neuropathy due to a granular cell tumor, who complained of foot dragging. Common peroneal neuropathy was confirmed by electrophysiology. The tumor mass was observed using ultrasonography and magnetic resonance imaging. The tumor was surgically excised, the tumor cells stained positive for S-100, and eosinophilic granular cytoplasm was observed using microscopy. To the best of our knowledge, this is the first report of a granular cell tumor involving the common peroneal nerve.
Granular cell tumors (GCTs) were first described by Abrikossoff in 1926, as “myoblastomas” [1,2], and recent studies have indicated they are derived from Schwann cells [1]. GCTs typically contain large, monotonous polygonal cells with abundant eosinophilic granular cytoplasm on microscopy and are mostly benign; however, a few are malignant [2]. GCTs are rare soft-tissue tumors that typically involve the skin and soft tissues of the head, neck, and trunk [3]. GCTs involving the peripheral nerves are rare [3,4] and, to our knowledge, GCTs arising from the common peroneal nerve have not been reported. Herein, we present the first reported case of a GCT of the common peroneal nerve.
A 35-year-old woman presented to our hospital with a 2-year history of progressively worsening right foot dragging. The motor power of the right ankle dorsiflexor and long toe extensor was measured as grades 1 and 2, respectively, on the Medical Research Council scale [5]. The motor power of the right ankle plantar flexion was graded as 5. There was no sensory loss in either lower extremity. On palpation of the right popliteal area, a tingling sensation was provoked in the anterior calf; however, there was no palpable mass.
This study was approved by the Institutional Review Board of Kangwon National University Hospital (2022-06-001) and requirement for informed consent was waived.
The common peroneal compound motor action potential (CMAP) was not obtainable in the right extensor digitorum brevis (EDB) and showed low amplitude in the right tibialis anterior (TA), with normal latency and conduction velocity (Table 1). In the sensory nerve conduction study, the nerve conduction velocity (NCV) of the right superficial peroneal nerve was slower than normal limit (39.8 m/sec) (Table 1). Skin temperature was measured at > 31°C during the study period.
Needle electromyography of the right lower extremity revealed abnormal spontaneous activities of the EDB and TA muscles at rest (Table 2). In the EDB, the motor units were not recruited with volition. In the TA, the motor unit action potentials were noted to be polyphasic and long-duration, and motor unit recruitment was reduced. No abnormalities were observed in the vastus medialis, gastrocnemius, abductor hallucis, short head of the biceps femoris, or peroneal longus.
Based on these findings, the possibility of deep peroneal neuropathy was initially considered. However, given the observed slowing of the NCV in the superficial peroneal nerve, the diagnosis was more closely suggestive of common peroneal neuropathy. Consequently, we concluded that the electrophysiological diagnosis for the patient was common peroneal neuropathy.
Ultrasonography (US) was performed using a GE LOGIQ P6 Pro (General Electric, Milwaukee, WI, USA) with a 3.42 to 10.85 MHz linear probe. The imaging revealed a hypoechoic oval mass with clear margins, measuring 4.0 × 1.0 cm2, on the lateral posterior region of the right knee (Fig. 1A, B). No vascularity of the mass was detected on Doppler US. Magnetic resonance imaging (MRI) revealed a well-circumscribed fusiform mass measuring 4.1 × 0.9 × 0.9 cm3. The mass exhibited similar signal intensity to the muscles on T1-weighted imaging (Fig. 1C) and showed high signal intensity on fat-suppressed T2-weighted imaging (Fig. 1D-F).
Both the US and MRI examinations indicated that the mass was located on the posterior side of the distal biceps femoris tendon and adjacent to the common peroneal nerve. These findings supported the electrophysiological diagnosis, which had suggested common peroneal neuropathy.
In a posterior right knee approach, a longitudinal skin incision was made on posterolateral aspect under spinal anesthesia. A yellowish fusiform mass encircling the common peroneal nerve below the biceps femoris muscle was noted (Fig. 2A). Although the mass could not be easily dissected from the common peroneal nerve, complete removal was achieved without nerve injury. The excised mass measured approximately 4 × 1 × 1 cm3 (Fig. 2B).
Ten months after surgery, a follow-up electrodiagnostic study showed a slight improvement in the peroneal CMAP amplitude (4.5 mV) compared to the initial examination (3.5 mV) recorded in the right TA; however, overall, there was no significant improvement in the strength of the right ankle.
GCTs rarely arise in the peripheral nerves and even more rarely in the lower extremities and, to our knowledge, no cases involving the common peroneal nerve have been reported [6]. The gradual onset of symptoms is often associated with a progressively growing mass around the common peroneal nerve [7]. An electrophysiological study can diagnose common peroneal neuropathy, but the underlying cause of neuropathy may be attributed to a mass (intraneural ganglion cyst) or tumors (schwannoma or neurofibroma) [7], and some may be malignant [2].
In certain cases, mass lesions in the deep popliteal region are not palpable [8]. However, in our case, although the mass was not palpable, palpating the popliteal fossa induced tingling sensations in the anterior calf. The positive Tinel sign supported the possibility of a lesion involving the common peroneal nerve of the popliteal area. Testing for the Tinel sign is a crucial physical examination technique when a mononeuropathy is suspected. A further imaging evaluation is necessary to differentiate the various potential causes of the lesion [8].
MRI of GCTs reveals quite different patterns between the soft tissue and peripheral nerves. GCTs occurring in the breast show unclear or irregular boundaries with the surrounding soft tissue [9], but GCTs occurring in the peripheral nerves appear as well-circumscribed masses with low or intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images, which is similar to our case [3,4,6].
US is a highly useful imaging modality for peripheral nerves because it is accessible at the bedside and can be used in conjunction with electromyography. No generally shared features of peripheral nerve GCTs have been described in previous reports. In the breast, a common site of GCT occurrence, the tumor presents as an irregular shape with hypoechoic or heteroechoic masses and ill-defined margins on US [9]. Intramuscular GCT was observed as an oval-shaped mass with inhomogeneous echogenicity and internal vascular signals on US [1]. The US features of GCTs in peripheral nerves have rarely been described. Qiyong et al. [3] described a GCT in the facial nerve; the tumor was irregular in shape, with hypoechogenicity, unclear borders, and blood flow signals. In our case, the tumor was oval and appeared as a hypoechoic mass with clear margins on US, which was compatible with the MRI features of a well-circumscribed fusiform mass.
Histological and immunohistochemical analyses are useful diagnostic tools for GCTs [4], which have distinct features such as polygonal cells with an intensely eosinophilic granular cytoplasm on microscopy [1,2,9]. Immunohistochemistry typically reveals positive staining for S-100 protein, nestin, inhibin, CD68, CD63, and neuron-specific enolase [1,2], suggesting that GCTs are derived from Schwann cells.
Most GCTs are benign, as in our case, but approximately 0.5% to 2.0% are malignant [2]. Benign GCTs have a good prognosis after surgical excision; however, malignant GCTs have a poor prognosis, with a mortality rate of 40% [2]. Malignant GCTs are characterized by large cells (> 5 cm), rapid growth, high recurrence, metastasis [2], and histologically increased cellularity with marked pleomorphism and increased mitotic activity [2,6]. Therefore, the possibility of malignancy should be considered.
In a few reports, there was symptom improvement after 9 to 14 months since surgical resection of a GCT in the peripheral nerve [3,4,10]. In our case, the ankle dorsiflexion power did not show an obvious change in 10 months after complete excision of the GCT without nerve injury, even though there was an increase in the peroneal CMAP amplitude in the motor nerve conduction study. The recurrence rate of GCT could be 2% to 8% in cases with clear resection margins, and up to 50% in cases where margins are unclear [4]. Long-term follow-up would be necessary to confirm the absence of recurrence and observe symptom improvement.
We present a patient who complained of progressive right foot dragging. Common peroneal neuropathy associated with an unpalpable mass lesion was assessed using electrophysiology, US, and MRI. The diagnosis of GCT was confirmed histologically after surgical excision. To the best of our knowledge, this is the first report of a GCT involving the common peroneal nerve. We believe that this case report will be helpful in the diagnosis of GCT of the common peroneal nerve.
Conflict of Interest
Sora Baek is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Fig. 1.
Ultrasonography (A, B) and magnetic resonance imaging (C-F) of the right knee. In the longitudinal view (A) and transverse view (B), a hypoechoic oval mass (*) was observed. A sagittal T1-weighted image (C), and sagittal (D), coronal (E), and axial T2-weighted (F) images demonstrated a well-circumscribed fusiform mass (white arrows) in the posterior side of the biceps femoris tendon. VL, vastus lateralis; BF, biceps femoris; GCM-L, lateral head of the gastrocnemius; ST, semitendinosus; GCM-M, medial head of the gastrocnemius.
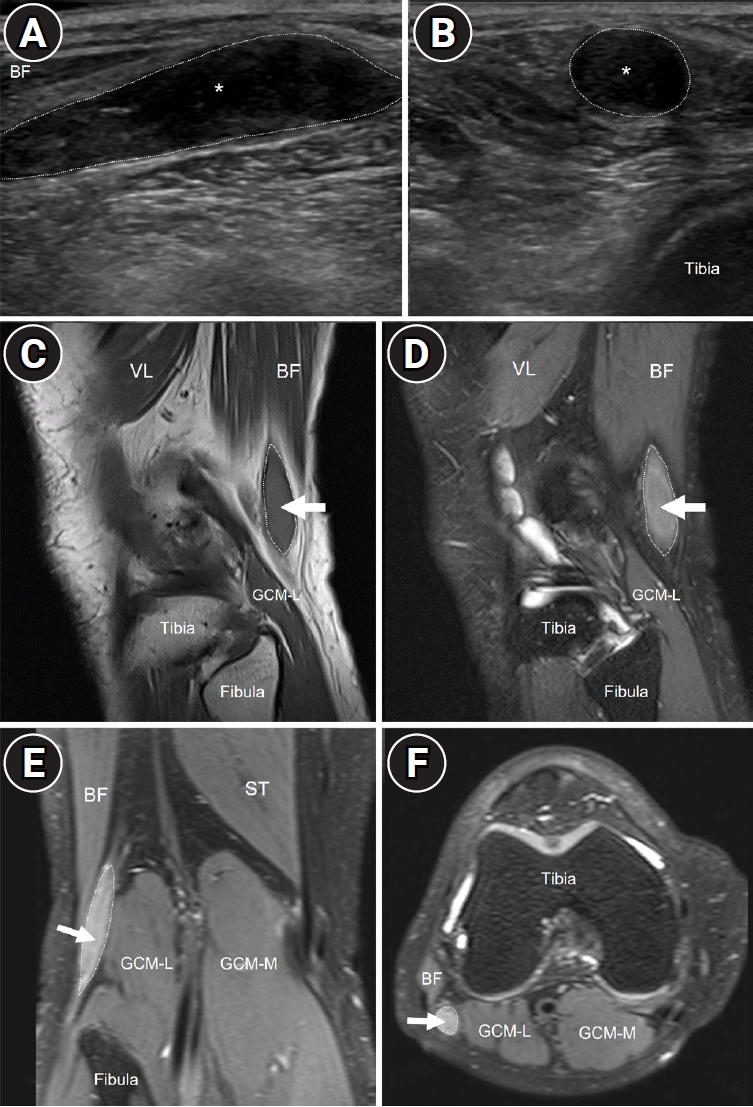
Fig. 2.
Intraoperative photograph. The image shows a yellowish, non-hard, fusiform mass (white arrow) adjacent to the common peroneal nerve (white arrowhead) (A), and the mass was totally dissected from the nerve (B).
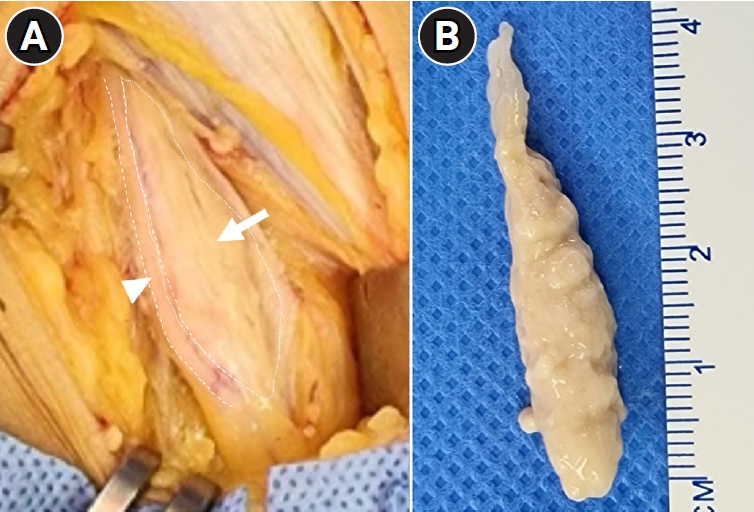
Fig. 3.
Histopathological and immunohistochemical examination of the excised tumor. Polygonal cells (black arrows) with a light pink granular eosinophilic cytoplasm and hyperchromatic nuclei (black arrowheads) on hematoxylin and eosin staining (A: × 200; B: × 400 magnification). Immunohistochemical analyses indicate that the tumor cells were strongly positive for CD68 protein (C: × 100 magnification) and S-100 protein (D: × 400 magnification).
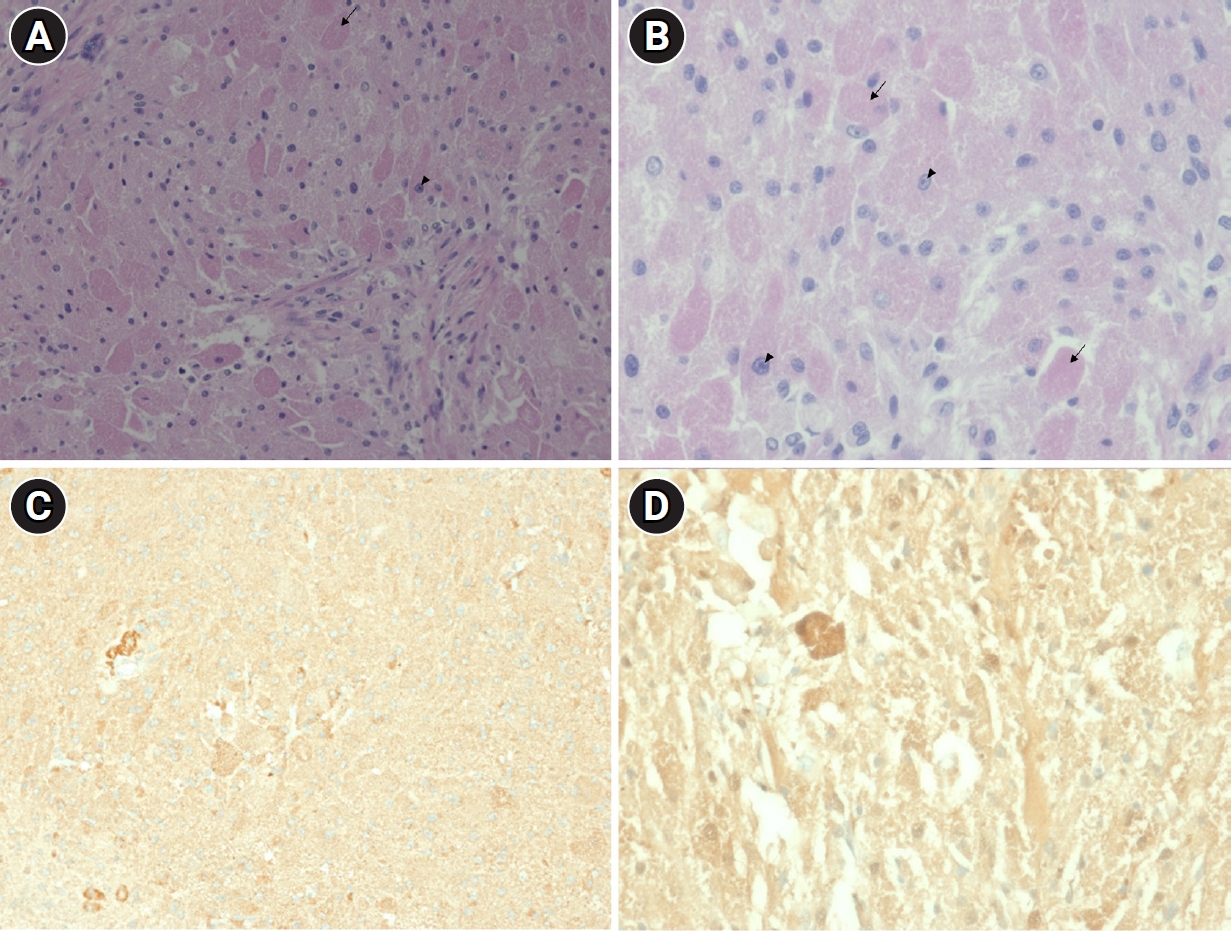
Table 1.
Nerve Conduction Study Findings
Table 2.
Needle Electromyography of the Right Lower Extremity
REFERENCES
1. Porta N, Mazzitelli R, Cacciotti J, Cirenza M, Labate A, Lo Schiavo MG, et al: A case report of a rare intramuscular granular cell tumor. Diagn Pathol 2015;10:162.



2. Singh VA, Gunasagaran J, Pailoor J: Granular cell tumour: malignant or benign? Singapore Med J 2015;56:513-517.



3. Qiyong Q, Qinying W, Quancheng L, Liang C, Haihong C: Granular cell tumor of the trunk of the facial nerve: a case report. Medicine (Baltimore) 2019;98:e15657.



4. Davis GA: Granular cell tumor: a rare tumor of the ulnar nerve: case report. Neurosurg Focus 2007;22:E25.


5. Medical Research Council: Aids to the investigation of the peripheral nervous system. London: Her Majesty’s Stationary Office, Medical Research Council; 1943.
6. Hurrell MA, McLean C, Desmond P, Tress BM, Kaye A: Malignant granular cell tumour of the sciatic nerve. Australas Radiol 1995;39:86-89.


7. Preston DC, Shapiro BE: Electromyography and neuromuscular disorders. 3rd ed. Philadelphia: Elsevier Inc.; 2013.

8. Kwon SW, Noh JS, Park JW, Sung DH, Kwon HK: Common peroneal neuropathy caused by intraneural ganglion cyst, electrophysiological findings related to fascicular involvement and operative findings in two cases. J Electrodiagn Neuromuscul Dis 2020;22:61-67.


-
METRICS

-
- 0 Crossref
- Scopus
- 861 View
- 17 Download
- Related articles in J Korean Assoc EMG Electrodiagn Med
-
Two Cases of Leigh Syndrome with Peripheral Neuropathy2008 June;10(1)






